Lifelong habits like musical training, reading, and handwriting help the brain stay efficient and resilient as we age.


In a Science Immunology Review from earlier this year, researchers discuss how interactions between the nervous and immune systems could impact neurological disorders and allergy-related behaviors like food avoidance.
The nervous and type 2 immune systems regulate each other via cytokines and neurotransmitters, suggesting previously unidentified therapeutic avenues.

Liu et al. report chromosome-level genomes of 11 species across 10 Polygonaceae genera (including four previously published genomes), which encompass diverse habitats. Integrating genomic and transcriptomic analyses, this study provides insights into the evolutionary adaptation strategies of Polygonaceae to thrive in various habitats.
Getting older means losing things. Some are fine, like any f**ks you have left to give or your tolerance for cheap tequila. Others, like the ability to follow a conversation in a loud room, hit harder.
But scientists now think there’s a way to fight back. And it might start at a piano bench.
Researchers publishing in PLOS Biology found that older adults who have played music for decades have brains that function more like those of someone half their age, at least when it comes to understanding speech in loud environments. In brain scans, they showed cleaner, more focused activity while listening to spoken syllables buried in background noise. Their brains weren’t scrambling. They already knew what to do.
Vascular aging and genetic risk jointly shape coronary artery disease susceptibility across races and sexes.
BackgroundEstimated pulse wave velocity (ePWV), a noninvasive marker of arterial stiffness, reflects vascular aging and has been associated with increased coronary artery disease (CAD) risk. However, the interplay between ePWV and genetic factors, including polygenic risk score (PRS) and apolipoprotein E genotypes, in determining CAD susceptibility remains unclear.

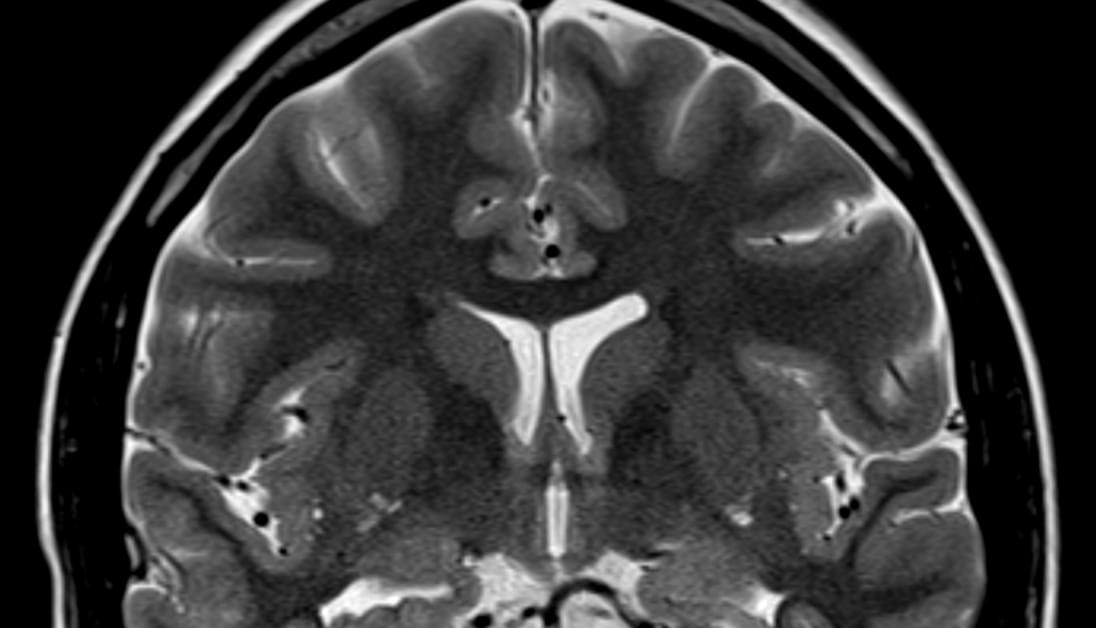
This review examines some of the monogenic disorders that can masquerade as neuroinflammatory phenotypes.
A recent explosion in genomic testing has led to the identification of several genetic disorders that mimic CNS-specific autoimmune disorders. Such monogenic disorders, although rare, represent a diagnostic challenge because of their diverse phenotypes and overlapping features. Early recognition of these disorders is crucial not only to prevent overtreatment with immunotherapy but also to ensure that targeted treatments are available for many of these disorders. This review explores some of the monogenic disorders that can masquerade as neuroinflammatory phenotypes. These clinical vignettes are stratified according to neuroanatomical localization along the neuroaxis: supratentorial white matter, gray matter, brainstem, and spinal cord involvement.


