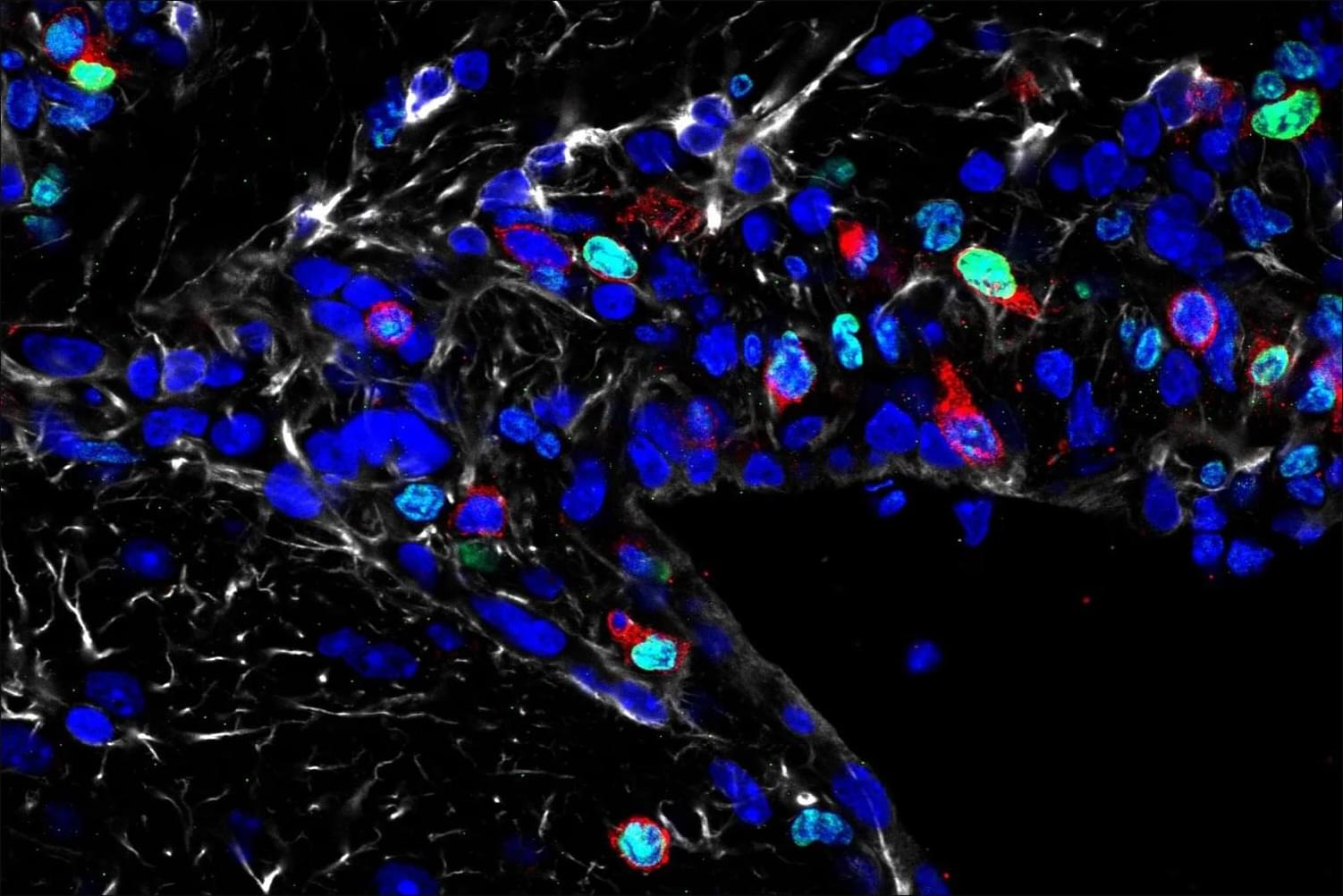
Cellular reprogramming is one of the technologies most associated with longevity. The field was created in 2006, when Shinya Yamanaka showed that a cocktail of four transcription factors, commonly known as OSKM, can cause de-differentiation and massive rejuvenation of a cell, creating an iPSC (induced pluripotent stem cell). About a decade later, partial reprogramming was demonstrated in vivo, where a more subtle application of the factors led to rejuvenation without compromising the cell’s identity.
Today, this field is maturing quickly, with its first clinical trials just around the corner. Academic teams and companies are working on dozens of directions and applications. We asked four experts, all involved in reprogramming-related biotech companies, to talk about their companies’ approaches and the opportunities and bottlenecks that the field faces and to offer predictions for the near and not-so-near future.
What I find most compelling about cellular reprogramming is that it revealed aging to be, at least in part, an actively maintained biological state rather than irreversible accumulation of damage. The discovery that somatic cells retain a latent capacity to reset their epigenetic and functional identity fundamentally changed how we think about cellular plasticity, identity, and time.