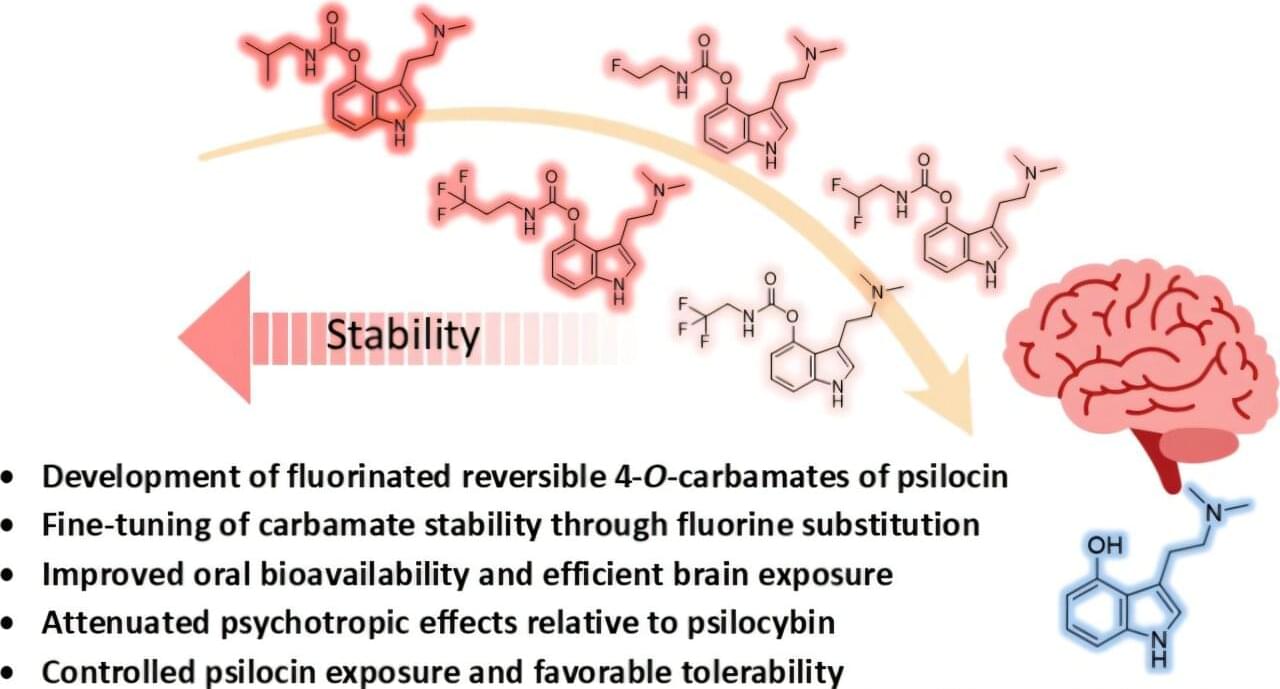
Psilocybin—the psychoactive compound in “magic mushrooms”—is gaining scientific attention for its potential in treating neuropsychiatric conditions including depression, anxiety, substance use disorders and certain neurodegenerative diseases. However, its hallucinogenic effects may limit broader therapeutic applications. Researchers publishing in the Journal of Medicinal Chemistry synthesized modified versions of psilocin, the active form of psilocybin, that retained its activity while producing fewer hallucinogenic-like effects than pharmaceutical-grade psilocybin in a preliminary study in mice.
“Our findings are consistent with a growing scientific perspective suggesting that psychedelic effects and serotonergic activity may be dissociated,” says Andrea Mattarei, a corresponding author of the study. “This opens the possibility of designing new therapeutics that retain beneficial biological activity while reducing hallucinogenic responses, potentially enabling safer and more practical treatment strategies.”
Mood disorders and some neurodegenerative diseases, such as Alzheimer’s disease, involve imbalances of the neurotransmitter molecule serotonin, which helps regulate mood and other brain functions. For decades, scientists have been investigating the therapeutic use of psychedelics such as psilocybin on serotonin-signaling pathways. However, the hallucinations that can accompany these drugs may make people wary of taking them, even if there is a medical benefit.