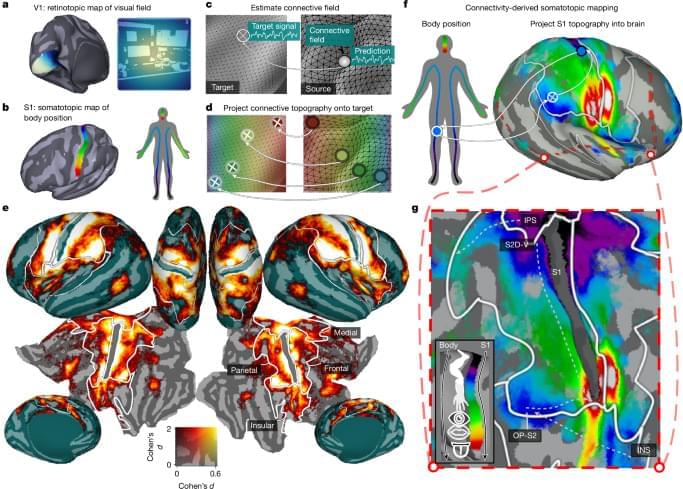
A central question in sensory neuroscience is how inputs from vision and touch are combined to generate cohesive representations of the external world. Here we reveal a widespread mode of brain organization in which aligned topographic maps bridge vision and somatosensation. We developed a computational model that revealed somatotopic structure in dorsolateral visual cortex. Somatotopic tuning in these regions was predictive of visual field locations more dorsally and visual body part selectivity more ventrally. These results suggest more extensive cross-modal overlap than traditionally assumed: the computational machinery classically attributed to the somatosensory system is also embedded within and aligned with that of the visual system. These aligned visual and bodily maps are a likely brain substrate for internalized somatosensory representations of visual signals, and are a candidate human homologue of findings in mice whereby somatomotor responses dominate visual cortex36.
Consistent with embodied perception theories, our model-based quantifications of somatotopic and retinotopic connectivity revealed that dorsolateral visual cortical responses to naturalistic stimuli are best explained by selectivities in both modalities, as opposed to visual selectivity alone. The necessity of incorporating body-referenced processing into models of dorsolateral visual cortex supports evidence that its role extends beyond passive visual analysis, encompassing perceptual, semantic and bodily functions optimized for behavioural interactions with the world25.
Consistent with visuospatial alignment of somatosensory tuning, we found that body part preferences in dorsolateral visual cortex predicted visual field tuning. Such alignment, previously reported at the terminus of the dorsal visual pathway around the postcentral sulcus28, therefore extends far into dorsal and lateral streams of the visual system. This alignment may be reinforced by shared developmental influences, as somatotopic and retinotopic maps are shaped trophically from birth: dorsal regions represent the upper body and visual field, and ventral regions to the lower body and visual field22, providing a roughly aligned sensory periphery optimized for efficient environmental sampling and action. The explicit interweaving of touch and retinal coordinates may subserve efficient perception of environmental affordances and a cohesive sense of spatial self-representation.