Scientists rebuilt human brain circuits in the lab and discovered that the thalamus acts as a central organizer of cortical wiring. The findings offer new insight into how brain networks form and why they sometimes go awry.
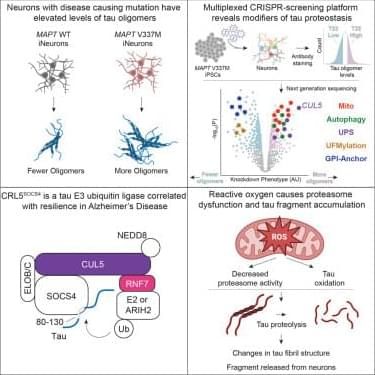
An investigation by researchers from Case Western Reserve University School of Medicine in the US has filled in a missing link between the toxic build-up of proteins in the neurodegenerative condition Parkinson’s disease and the death of critical brain cells.
The result of three years of research, the discovery connects alpha-synuclein proteins to a breakdown in mitochondrial function, both previously linked to Parkinson’s.
“We’ve uncovered a harmful interaction between proteins that damages the brain’s cellular powerhouses, called mitochondria,” says neuroscientist Xin Qi.
In the group treated with psilocybin, adapting neurons sat at a resting voltage that was closer to the threshold for firing. This state is known as depolarization. It means the cells are primed to activate more easily. The bursting neurons in psilocybin-treated rats also showed increased excitability. They required less input to trigger a signal and fired at faster rates than neurons in untreated rats.
The rats treated with 25CN-NBOH also exhibited functional changes, though the specific electrical alterations differed slightly from the psilocybin group. For instance, the bursting neurons in this group were not as easily triggered as those in the psilocybin group. However, the overall pattern confirmed that the drug had induced a lasting shift in neuronal function.
These electrophysiological findings provide a potential explanation for the behavioral results. While the physical branches of the neurons may have pruned back to normal levels, the cells “remembered” the treatment through altered electrical tuning. This functional shift allows the neural circuits to operate differently long after the drug has left the body.
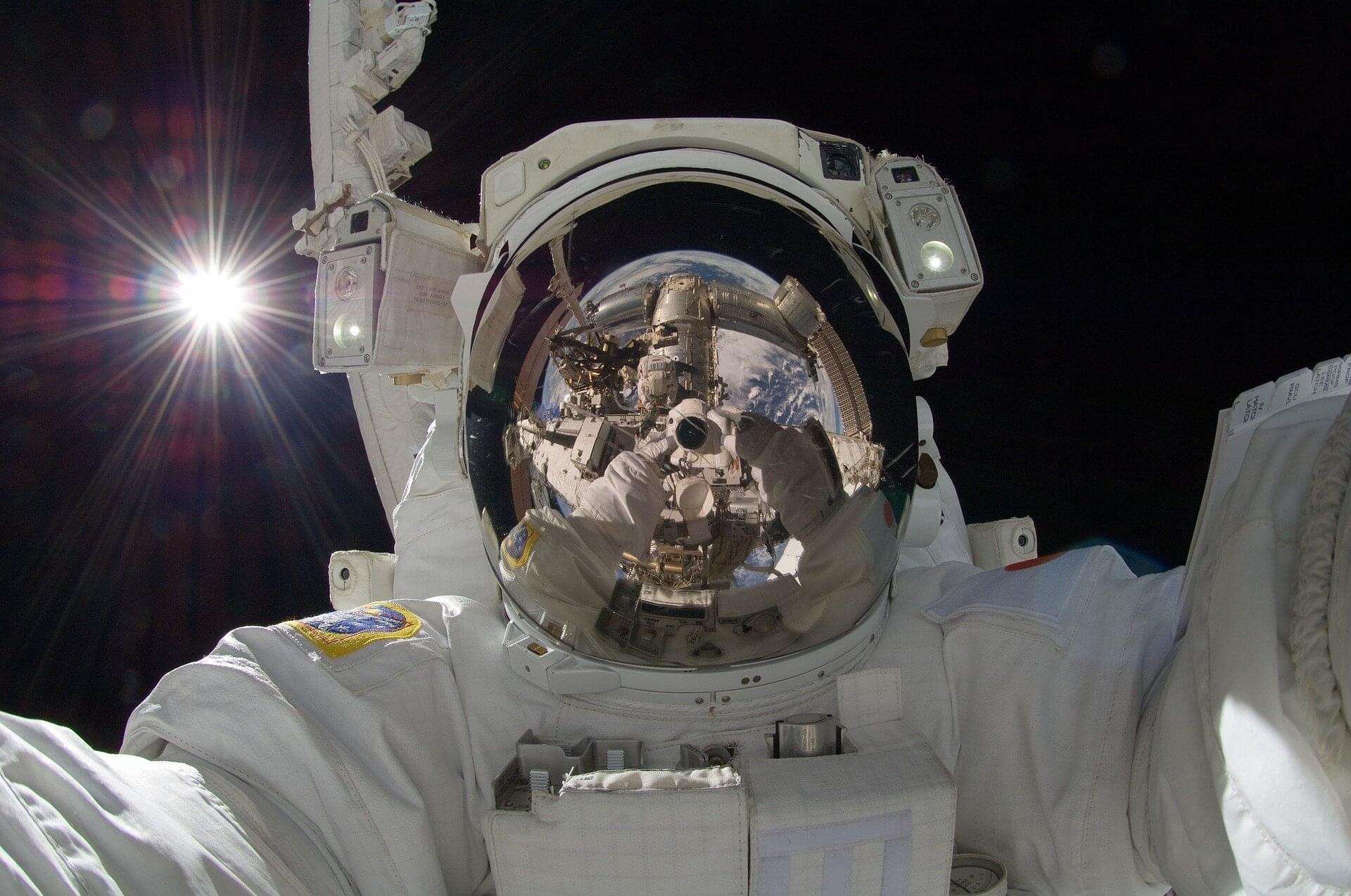
Spaceflight takes a physical toll on astronauts, causing muscles to atrophy, bones to thin and bodily fluids to shift. According to a new study published in the journal PNAS, we can now add another major change to that list. Being in microgravity causes the brain to change shape.
Here on Earth, gravity helps to keep the brain anchored in place while the cerebrospinal fluid that surrounds it acts as a cushion. Scientists already knew that, without gravity’s steady pull, the brain moves upward, but this new research showed that it is also stretched and compressed in several areas.
Brains on the move Researchers led by Rachel Seidler at the University of Florida reached this conclusion after studying MRI scans of 26 astronauts taken before and after their missions to the International Space Station. These were compared with scans from 24 volunteers who participated in a head-down tilt bed rest experiment. They spent 60 days lying at a six-degree downward angle to mimic how weightlessness causes bodily fluids and organs to move toward the head.
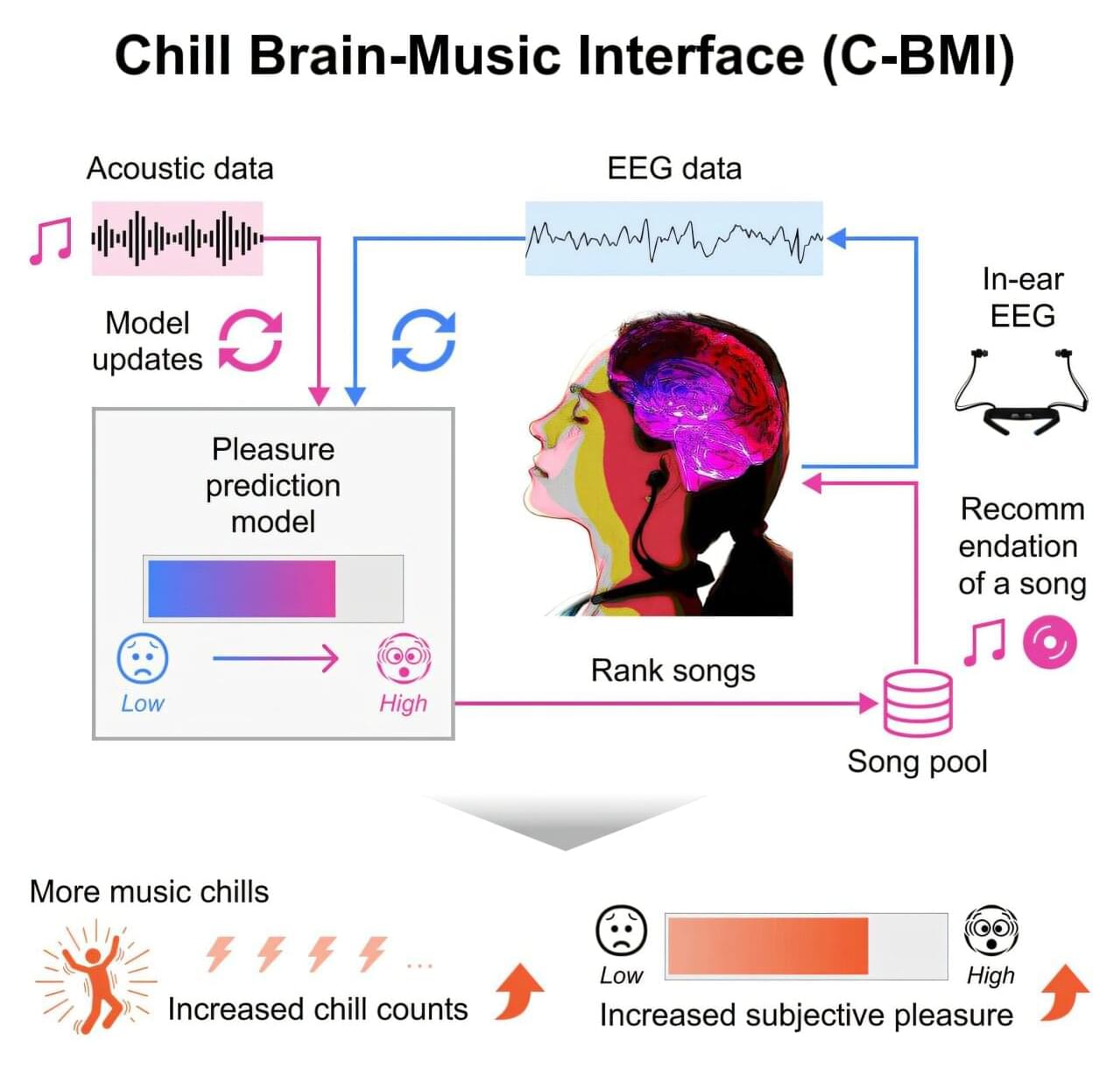
Musical chills are pleasurable shivers or goosebump sensations that people feel when they resonate with the music they’re listening to. They reduce stress and have beneficial side effects, but they are difficult to induce reliably. Now, researchers from Japan have developed a practical system that uses in-ear electroencephalography sensors to measure the brain’s response to music in real time and provide music suggestions that enhance chills.
Most people are familiar with “musical chills”—a sudden, involuntary shiver or goosebump sensation that occurs when a song resonates perfectly with one’s emotions. These chills are not just a surface-level feeling, but a profound neurological event. When we experience intense musical pleasure, parts of the brain’s reward system activate in a manner similar to how they would respond to life-affirming stimuli, such as beloved foods or positive social connections.
However, despite the universal nature of the experience, musical chills are difficult to trigger reliably. This limits our ability to harness their psychological and physiological benefits, even with today’s on-demand access to vast libraries of music.

Hey everyone! I wrote a proposal on creating massively scalable gene therapy delivery systems towards unlocking cures for widespread debilitating psychiatric diseases! Would love for folks to take a read and provide constructive suggestions to iterate this vision. [ https://substack.com/home/post/p-186453159]
Restoring joy to a billion lives.

Deco et al. used neurotransmission-modulated (NEMO) whole-brain modeling to flexibly compute a broad repertoire of empirical tasks and associated neuroimaging data from 971 healthy participants. NEMO can sculpt the different brain dynamics in a fixed brain architecture to compute the rich repertoire of tasks required for surviving and thriving.