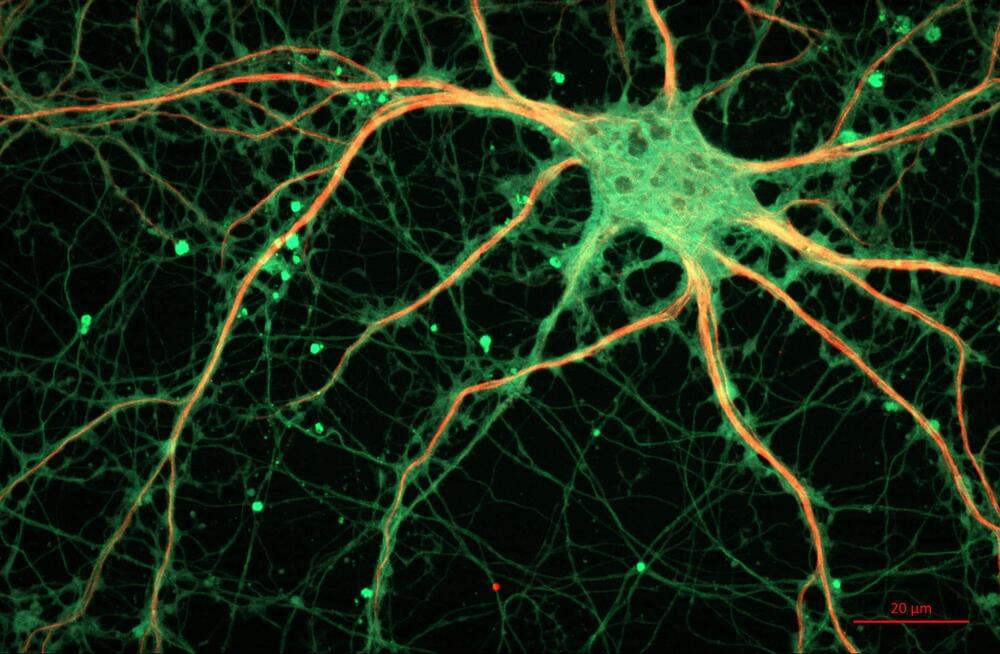
A University of Minnesota Twin Cities-led team has found that electrical stimulation of the body combined with sound activates the brain’s somatosensory or “tactile” cortex, increasing the potential for using the technique to treat chronic pain and other sensory disorders. The researchers tested the non-invasive technique on animals and are planning clinical trials on humans in the near future.
The paper is published in the Journal of Neural Engineering, a highly regarded, peer-reviewed scientific journal for the interdisciplinary field of neural engineering.
During the experiments, the researchers played broadband sound while electrically stimulating different parts of the body in guinea pigs. They found that the combination of the two activated neurons in the brain’s somatosensory cortex, which is responsible for touch and pain sensations throughout the body.