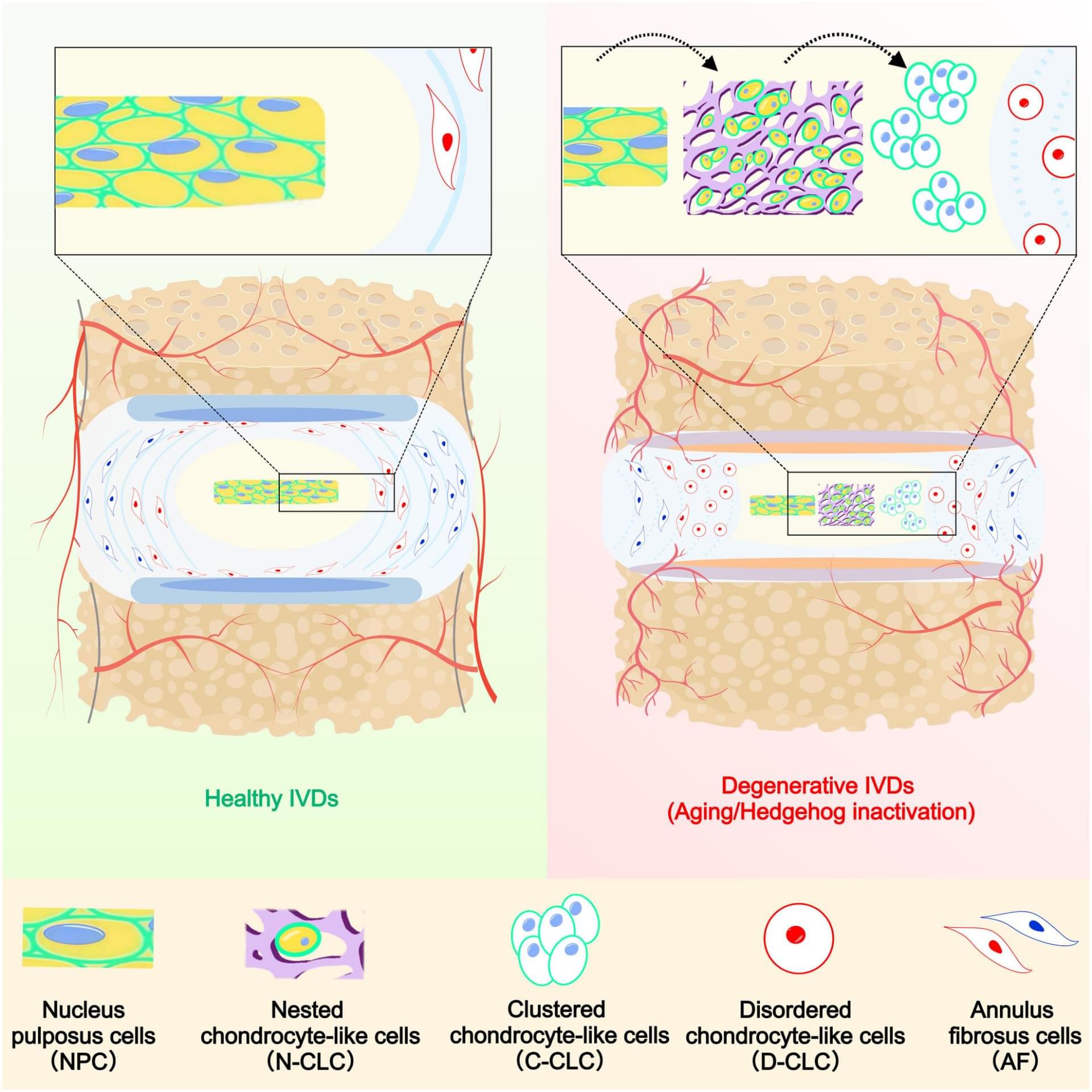
During intervertebral disc degeneration, notochord-derived nucleus pulposus cells progressively transdifferentiate into Krt19+ chondrocyte-like cells (CLCs) and Krt19− CLCs, which are eventually repl…
Join us on Patreon! https://www.patreon.com/MichaelLustgartenPhD
Discount Links/Affiliates:
Blood testing (where I get the majority of my labs): https://www.ultalabtests.com/partners/michaellustgarten.
At-Home Metabolomics: https://www.iollo.com?ref=michael-lustgarten.
Use Code: CONQUERAGING At Checkout.
Clearly Filtered Water Filter: https://get.aspr.app/SHoPY
Epigenetic, Telomere Testing: https://trudiagnostic.com/?irclickid=U-s3Ii2r7xyIU-LSYLyQdQ6…M0&irgwc=1
Use Code: CONQUERAGING
NAD+ Quantification: https://www.jinfiniti.com/intracellular-nad-test/
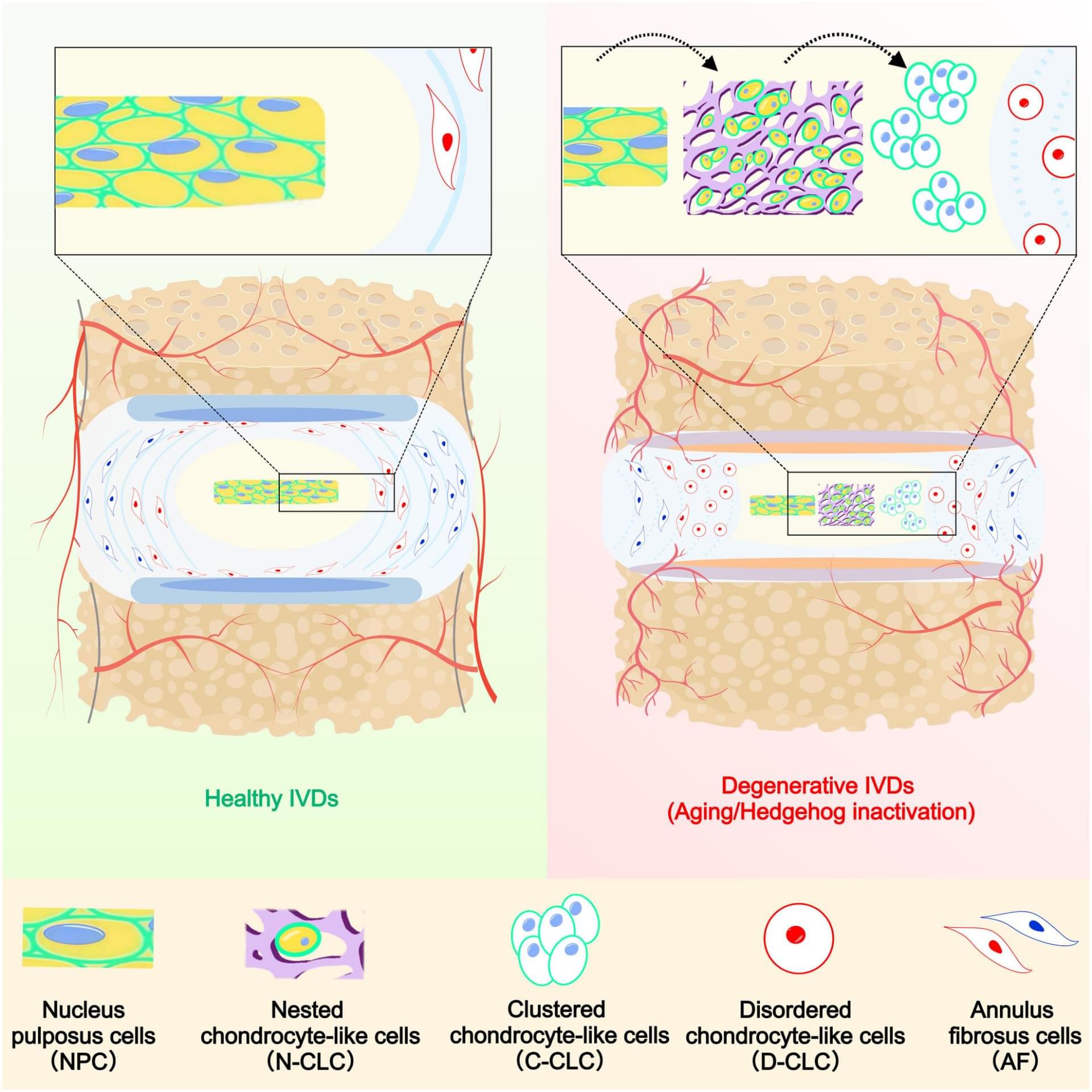
Research led by The Hong Kong Polytechnic University finds that regional fat distribution exerts distinct effects on brain structure, connectivity and cognition, revealing patterns not explained by body mass index (BMI).
Obesity has been associated with structural and functional changes in the brain, including reductions in gray matter, disruptions in white matter and impaired connectivity, which have been associated with cognitive decline.
Previous studies frequently used BMI as the central measure of obesity, a highly generalized metric that cannot capture the biological differences in fat depots. Adipose tissue in different body regions is known to affect metabolic and inflammatory pathways differently, and earlier work has suggested that visceral (around organs in the abdominal cavity) and leg fat contribute unequally to disease risk.
Conquering aging via TRCS — the telomere DNA AND ribosomal DNA co-regulation model for cell senescence — bilu huang — CSO, fuzhuang therapeutics.
Bilu Huang (https://biluhuang.com/) is a visionary scientist dedicated to finding solutions to some of the most pressing challenges facing humanity. His interdisciplinary work spans multiple fields, including biological aging, dinosaur extinction theories, geoengineering for carbon removal, and controlled nuclear fusion technology.
Born in Sanming City, Fujian Province, Huang is an independent researcher whose knowledge is entirely self-taught. Driven by curiosity and a relentless pursuit of scientific exploration, he has achieved numerous research results through his dedication and passion for science.
As a talented theoretical gerontologist, he proposed the Telomere DNA and ribosomal DNA co-regulation model for cell senescence (TRCS) and he is now using this latest theory to develop biotechnology to rejuvenate cells which will be used to completely cure various age-related degenerative diseases and greatly extend human life at Fuzhuang Therapeutics (https://lab.fuzhuangtx.com/en/).
#Aging #Longevity #BiluHuang #FuzhuangTherapeutics #TelomereDNAAndRibosomalDNACoRegulationModelForCell #Senescence #TRCS #DinosaurExtinctionResearch #CarbonRemovalTechnology #ControlledNuclearFusion #TelomereDNA #RibosomalDNA #CellularAging #GeneticProgram #Telomere #P53
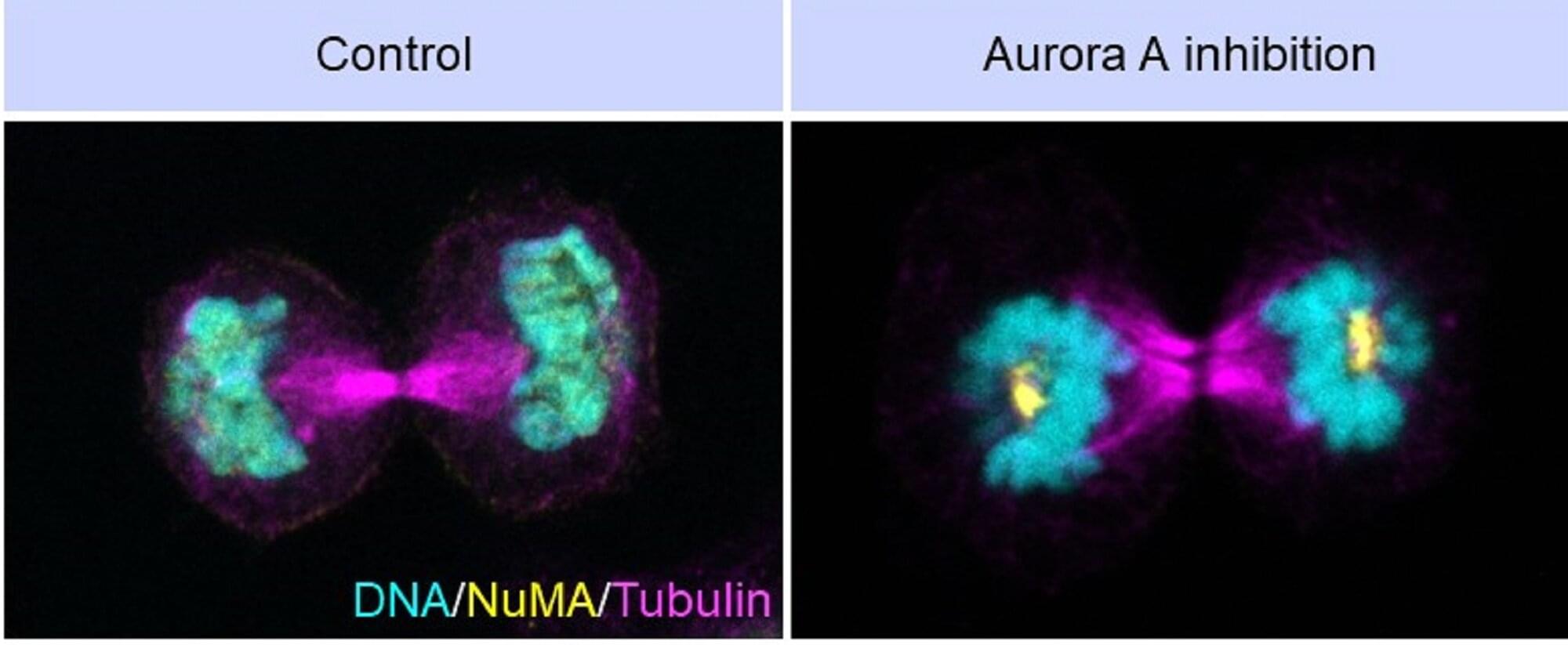
Every time a eukaryotic cell divides, it faces a monumental challenge: It must carefully duplicate and divide its genetic material (chromosomes) equally, and then rebuild the nuclear envelope around the separated halves. If this process goes wrong, the resulting nuclei can be misshapen or disorganized—features often seen in cancer and aging-related diseases.
A new study from researchers at the Indian Institute of Science (IISc) and Université Paris-Saclay reveals how a key enzyme called Aurora A helps cells pull off this feat. The findings are published in The EMBO Journal.
In dividing cells, structures called spindle poles (or centrosomes) grow in size to generate the microtubule ‘tracks’ that pull chromosomes apart. Once this job is done, the spindle poles must shrink and disassemble so that the nuclear envelope can reform around the separated chromosomes.

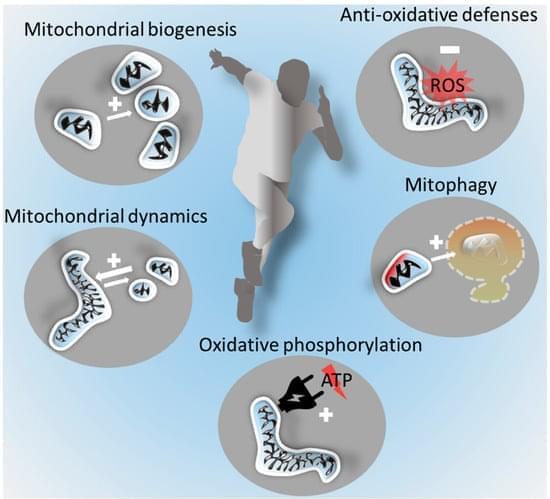
Regular exercise is associated with pronounced health benefits. The molecular processes involved in physiological adaptations to exercise are best understood in skeletal muscle. Enhanced mitochondrial functions in muscle are central to exercise-induced adaptations. However, regular exercise also benefits the brain and is a major protective factor against neurodegenerative diseases, such as the most common age-related form of dementia, Alzheimer’s disease, or the most common neurodegenerative motor disorder, Parkinson’s disease. While there is evidence that exercise induces signalling from skeletal muscle to the brain, the mechanistic understanding of the crosstalk along the muscle–brain axis is incompletely understood. Mitochondria in both organs, however, seem to be central players.

University of Oxford-led research finds low-dose rapamycin functions as a genomic protector in aging human immune cells, lowering DNA damage.
The mechanistic target of rapamycin (mTOR) is a central signaling pathway that regulates and coordinates cell growth, metabolism, and survival in response to environmental cues. It helps cells integrate signals from growth factors, nutrients, and stress to control whether they are in an anabolic (building up) or catabolic (breaking down) state.
Aging immune systems accumulate DNA damage linked to immunosenescence. Rapamycin is a drug that inhibits the mTOR pathway. Originally developed for organ transplantation to prevent immune rejection, previous research has found that, at non-immunosuppressive doses, rapamycin can mitigate cellular senescence.
Space isn’t just for lonely colonies—it’s for communities. Join us as we imagine constellations of space habitats bound by tethers, trade, and trust, building not just homes in the stars but entire civilizations.
Watch my exclusive video The Economics of Immortality: https://nebula.tv/videos/isaacarthur–…
Get Nebula using my link for 40% off an annual subscription: https://go.nebula.tv/isaacarthur.
Get a Lifetime Membership to Nebula for only $300: https://go.nebula.tv/lifetime?ref=isa…
Use the link https://gift.nebula.tv/isaacarthur to give a year of Nebula to a friend for just $36.
Visit our Website: http://www.isaacarthur.net.
Join Nebula: https://go.nebula.tv/isaacarthur.
Support us on Patreon: / isaacarthur.
Support us on Subscribestar: https://www.subscribestar.com/isaac-a…
Facebook Group: / 1583992725237264
Reddit: / isaacarthur.
Twitter: / isaac_a_arthur on Twitter and RT our future content.
SFIA Discord Server: / discord.
Credits:
Space Habitat Clusters & Conglomerations.
Written, Produced & Narrated by: Isaac Arthur.
Graphics: Jarred Eagley, Jeremy Jozwik, Udo Schroeter.
Select imagery/video supplied by Getty Images.
Music Courtesy of Stellardrone and Epidemic Sound http://epidemicsound.com/creator.
Chapters.
0:00 Intro.
1:13 Why Clustered Habitats?
6:00 Habitat Types and Roles Within Clusters.
9:41 Mobility and Modularity – The Politics of Moveable Worlds.
14:02 Tethers, Transit, and Shared Infrastructure.
17:35 Shapes of Clusters and Dynamic Conglomerations.
23:43 Nebula.
25:21 Digital Ecosystems and Cultural Identity.
25:19 Economics and Trade in Habitat Constellations.
26:52 Education and Intergenerational Planning.
28:17 Security and Conflict Management.
29:10 A Tale of Unity.
32:29 Religion, Ritual, and Meaning.
33:19 The Long View: Legacy and Civilization.
34:07 Closing Reflections