Sanofi’s apparent readiness to favour the US market with any Covid-19 vaccine caused a row in France.


The Plasma Protein Therapeutics Association (PPTA) and its member companies are closely monitoring the rapidly changing information landscape regarding the spread of Novel Coronavirus 2019 (COVID-19) and wish to be a resource for patients, plasma donors, policymakers, and other stakeholders during this pandemic.
Plasma donors save lives! Your donations are even more essential during the current COVID-19 pandemic to ensure patients with rare diseases can keep receiving their lifesaving treatments. Authorities in the U.S. and in the EU have published guidance documents recognizing the essential nature of plasma donation. Please click here to find a plasma donation center near you.
Training, Inference, Data Analytics Unified on One Platform; Each System Configurable from One to 56 Independent GPUs to Deliver Elastic, Software-Defined Data Center Infrastructure.
GTC 2020 — NVIDIA today unveiled NVIDIA DGX™ A100, the third generation of the world’s most advanced AI system, delivering 5 petaflops of AI performance and consolidating the power and capabilities of an entire data center into a single flexible platform for the first time.

Scientists have discovered a new treatment to dramatically reduce swelling after brain and spinal cord injuries, offering hope to 75 million victims worldwide each year.
The breakthrough in treating such injuries—referred to as central nervous system (CNS) edema—is thought to be hugely significant because current options are limited to putting patients in an induced coma or performing risky surgery.
Brain and spinal cord injuries affect all age groups. Older people are more at risk of sustaining them from strokes or falls, while for younger age groups, major causes include road traffic accidents and injuries from sports such as rugby, US-style football and other contact games.
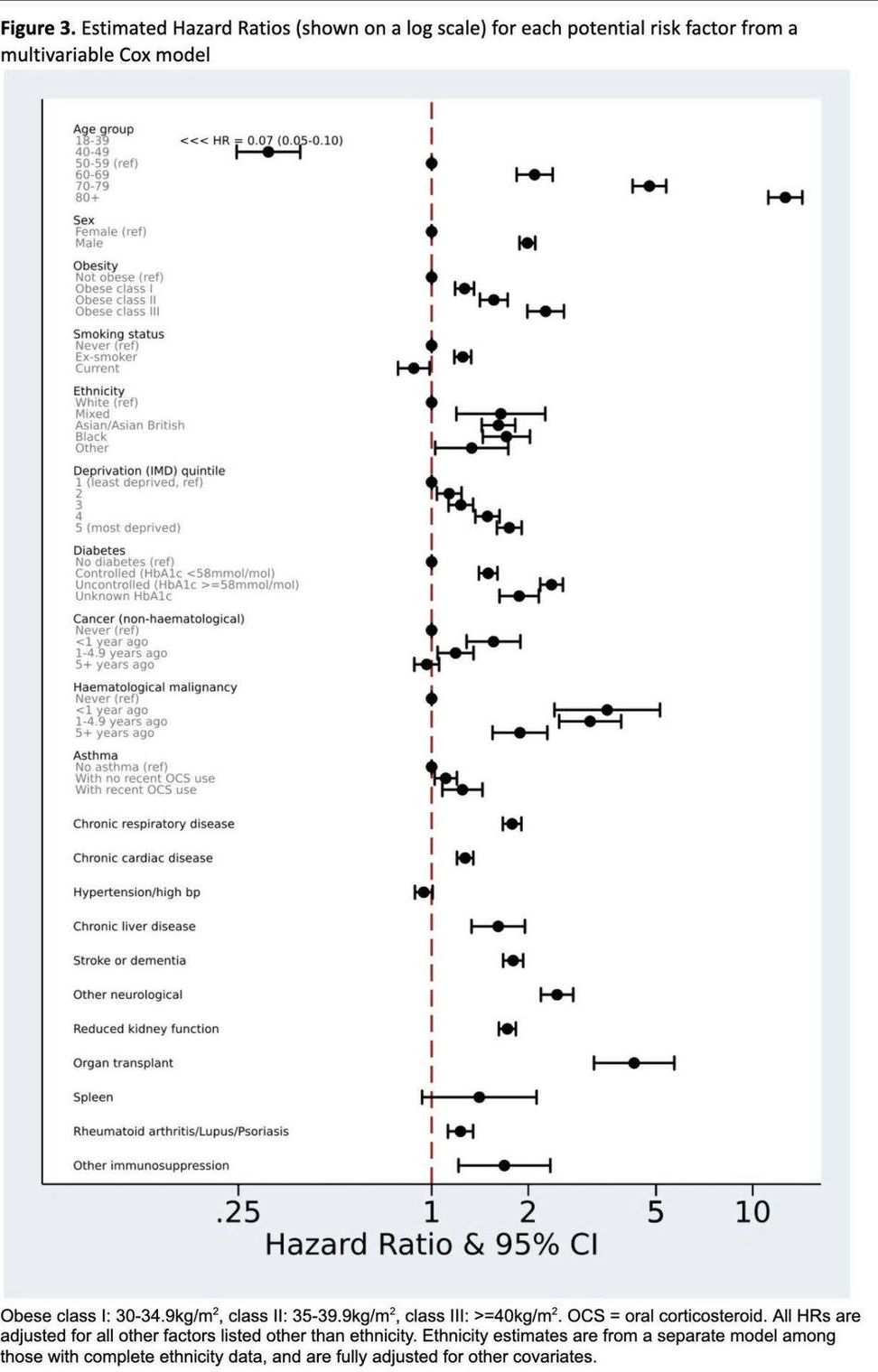
The largest study yet on COVID-19 fatality shows top risks:
Age, BY FAR the highest 2. Cancers of the blood 3. Male 4. Obesity 5. Diabetes.
I will say it again: Aging is a disease & it is treatable. Yes, treatable. Source: https://buff.ly/2LgK8Ya
Note that these are independent risk factors. If you are 65 and healthy, you are still at risk of dying from COVID- 19. Why? It could be that your cells have lost information. But lost information is recoverable, like a reboot. Source: https://buff.ly/2uhPtZJ
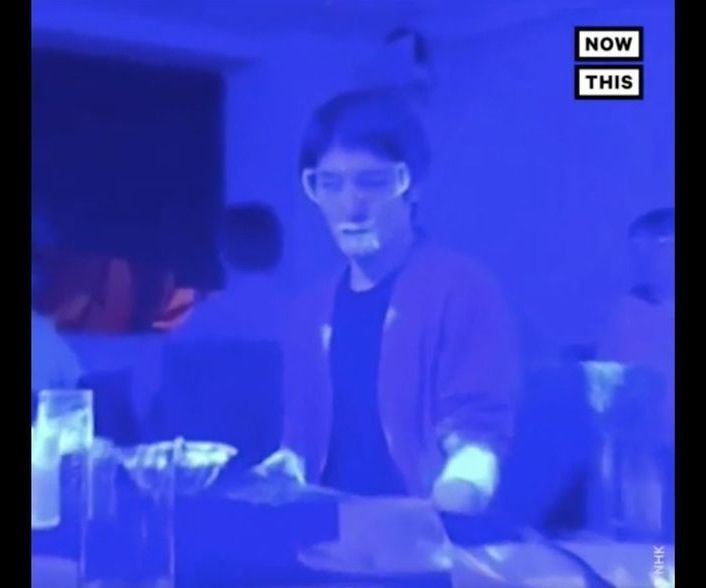
In the video, one person is designed as the “infected” patient and is given a special black light-ready solution to rub into his hands. (The solution is invisible without a black light, so participants in the demonstration can’t see it during the simulation.) Then, everyone in the experiment does what people normally do at a buffet restaurant — they dish up food, eat chat, and drink. At the end of the video, a black light is turned on, and you can see the “virus” just about everywhere. It shows up on utensils, cups, food and even on some participants’ faces.
Experts say this is definitely worth paying attention to.
“This is an accurate illustration of how many commonly touched surfaces there are and how many opportunities there are for viruses to spread,” Dr. Amesh A. Adalja, senior scholar at the Johns Hopkins Center for Health Security, tells Yahoo Life.

University of Alberta researchers are racing against the clock to test an antiviral drug that has been proven to cure a cat coronavirus and is hoped to have the same effect on people with COVID-19.
“Our lab has been working as fast as we can to get our results out,” said biochemist Joanne Lemieux. “We have not taken weekends, the days of the week have blurred. We’re all working non-stop to get results as fast as we can.”
The project is one of 11 at the U of A to receive funding from the federal government’s $52.6 million investment in COVID-19 research.
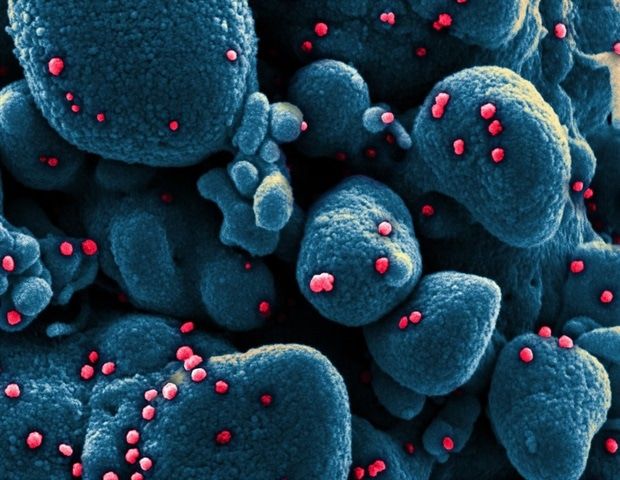
Joanne Lemieux and colleagues say the dipeptide-based protease inhibitor, GC376, and its analog, GC373, should be fast-forwarded for testing in clinical trials of COVID-19. The research is published on the preprint server bioRxiv*.
“They are strong drug candidates for the treatment of human coronavirus infections because they have already been successful in animals (cats),” writes the team. “The work here lays the framework for their use in human trials for the treatment of COVID-19.”
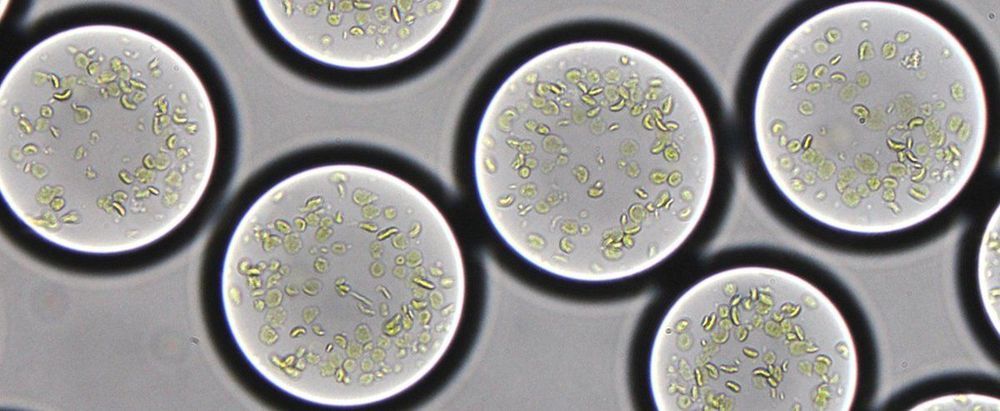
Over billions of years, microorganisms and plants evolved the remarkable process we know as photosynthesis. Photosynthesis converts sun energy into chemical energy, thus providing all life on Earth with food and oxygen. The cellular compartments housing the molecular machines, the chloroplasts, are probably the most important natural engines on earth. Many scientists consider artificially rebuilding and controlling the photosynthetic process the “Apollo project of our time.” It would mean the ability to produce clean energy—clean fuel, clean carbon compounds such as antibiotics, and other products simply from light and carbon dioxide.
But how to build a living, photosynthetic cell from scratch? Key to mimicking the processes of a living cell is to get its components to work together at the right time and place. At the Max Planck Society, this ambitious goal is pursued in an interdisciplinary multi-lab initiative, the MaxSynBio network. Now the Marburg research team led by director Tobias Erb has succeeded successfully created a platform for the automated construction of cell-sized photosynthetically active compartments, “artificial chloroplasts,” that are able to capture and convert the greenhouse gas carbon dioxide with light.
