Early results from the first COVID-19 vaccine candidate tested in people showed that it triggered an immune response against the virus with no serious side effects.
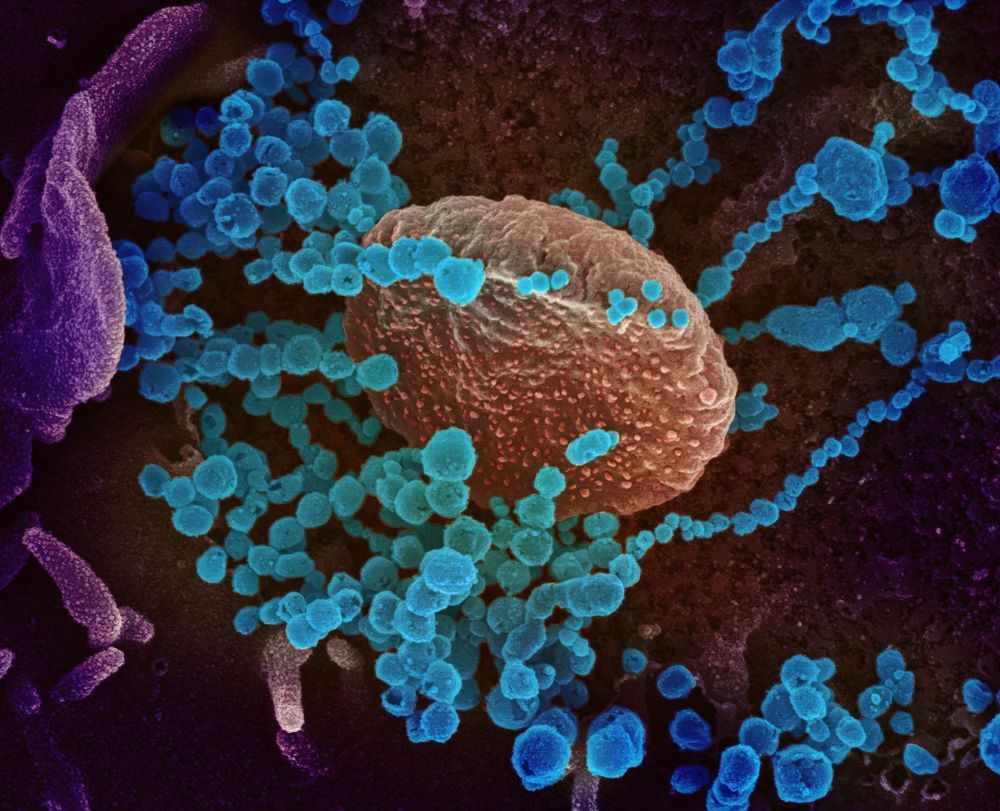

Featured image source: NASA / spacex
Axiom Space Inc. is a Houston, Texas start-up, founded by Michael Suffredini who served as NASA’s International Space Station (ISS) Program Manager from 2005 to 2015. He was responsible for overseeing ISS transition from assembly to the initiation of commercial operations. Axiom is mostly staffed by NASA ex-employees, including former NASA Administrator Charles Bolden. – “The leadership team also includes world-class, specialized expertise in commercial utilization of microgravity, on-orbit operations, astronaut training, space financing, engineering, space system architecture/design/development, space medicine, marketing, and law,” the company states. Together, they are all working towards the commercialization of space.
Axiom aims to build a space station in low Earth orbit to continue operations once NASA retires the ISS program and moves beyond the orbiting laboratory to focus operations on the lunar surface. The company also offers spaceflights for regular civilians to experience microgravity and amazing views of Earth from ISS. “While making access to Low Earth Orbit global during the remainder of ISS’ lifetime, Axiom is constructing the future platform that will serve as humanity’s permanently growing home, scientific and industrial complex in Low Earth Orbit (LEO) – the cornerstone of human activity in space,” company states on its website.
From diagnostics to treatments and vaccines, nanotechnology is being developed and deployed to help stop the spread of COVID-19.
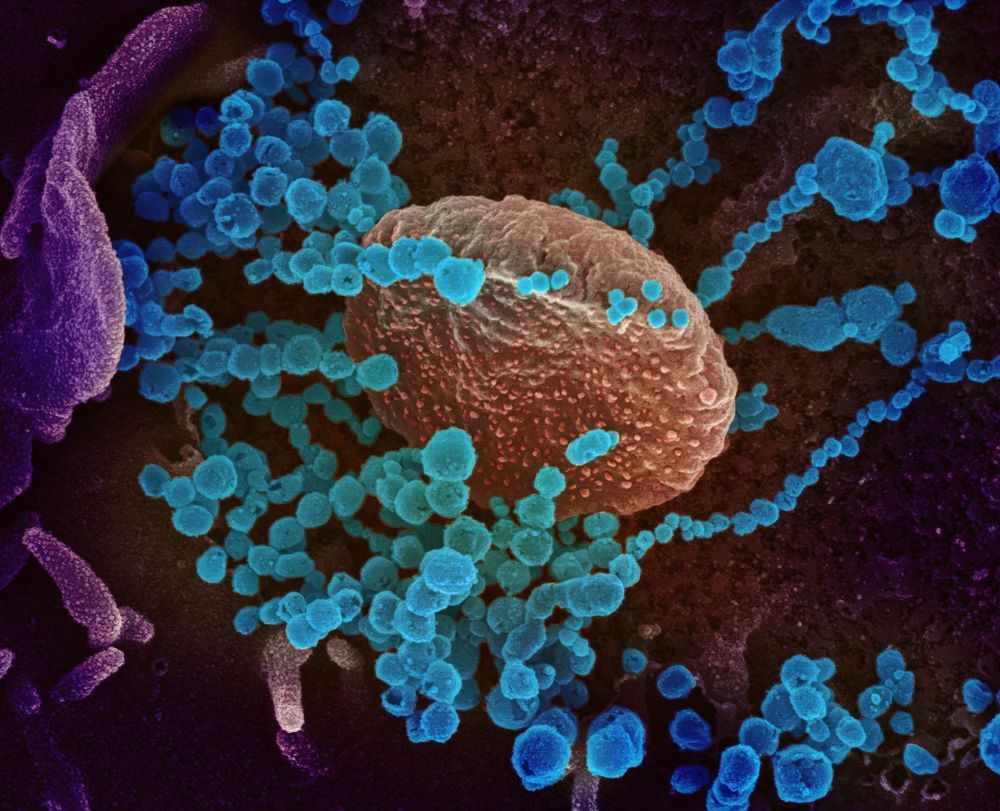
The world-altering coronavirus behind the COVID-19 pandemic is thought to be just 60 nanometres to 120 nanometres in size. This is so mind bogglingly small that you could fit more than 400 of these virus particles into the width of a single hair on your head. In fact, coronaviruses are so small that we can’t see them with normal microscopes and require much fancier electron microscopes to study them. How can we battle a foe so minuscule that we cannot see it?
The views expressed in this article are those of the author alone and not the World Economic Forum.

Who are we? Where did we come from? How did we get here? Throughout the ages, humans have sought answers to these questions, pursuing wisdom through religion, philosophy, and eventually science. Evolutionary analyses published by Genome Biology and Evolution (GBE) allow us to peer into the mirror and better understand ourselves as a species, bringing us closer than ever to uncovering the answers to these long-held questions. GBE’s latest virtual issue on human genetics highlights some of the most exciting research published in the journal within the last year and a half, demonstrating the wide variety of evolutionary approaches to this avenue of research as well as a number of fascinating insights into our own biology.
Taking over a decade to complete, the original Human Genome Project cost nearly $3 billion and involved the collective effort of hundreds of scientists. Since then, advances in sequencing technology have resulted in an explosion in human genetics and genomics research, with an estimated one million human genomes sequenced to date. While this wealth of data has the potential to answer some of our most fundamental questions, unlocking its mysteries has necessitated the invention of new analytic and computational methods and the integration of techniques and ideas from diverse biological sciences, including physiology, anatomy, medicine, population genetics, bioinformatics, and computational, molecular, and evolutionary biology.
A key area of investigation involves identifying ways in which humans differ from other primates—in other words, what makes us human? Several studies published over the last 18 months suggest that part of the answer may be found in transcriptional regulation and changes in gene expression. Edsall et al. (2019) evaluated differences in chromatin accessibility, which impacts access of the transcriptional machinery to the DNA, across five primates including humans. They found high levels of differentiation across species, as well as classes of sites that differed based on selection, genomic location, and cell type specificity. More specifically, Swain-Lenz et al. (2019) found that differences in chromatin accessibility near genes involved in lipid metabolism may provide a mechanistic explanation for the higher levels of body fat observed in humans compared to other primates. Arakawa et al.
Interesting technology looking to revolutionize both medical imaging and brain computer interfacing.
Han from WrySci HX explains the amazing Openwater system, which could rival Neuralink in the Brain Machine Interface space. More below ↓↓↓
Support 🙏
Patreon: https://www.patreon.com/wrysci_hx
OnlyFans: https://onlyfans.com/han_xavier
Subscribe! =]
Timestamp:

CIEQSFTTLFACQTAAEIWRAFGYTVKIMVDNGNCRLHVC: these forty letters are a set of instructions for building a sophisticated medical device designed to recognize the flu virus in your body. The device latches onto the virus and deactivates the part of it that breaks into your cells. It is impossibly tiny—smaller than the virus on which it operates—and it can be manufactured, in tremendous quantities, by your own cells. It’s a protein.
Proteins—molecular machines capable of building, transforming, and interacting with other molecules—do most of the work of life. Antibodies, which defend our cells against invaders, are proteins. So are hormones, which deliver messages within us; enzymes, which carry out the chemical reactions we need to generate energy; and the myosin in our muscles, which contract when we move. A protein is a large molecule built from smaller molecules called amino acids. Our bodies use twenty amino acids to create proteins; our cells chain them together, following instructions in our DNA. (Each letter in a protein’s formula represents an amino acid: the first two in the flu-targeting protein above are cysteine and isoleucine.) After they’re assembled, these long chains crumple up into what often look like random globs. But the seeming chaos in their collapse is actually highly choreographed. Identical strings of amino acids almost always “fold” into identical three-dimensional shapes. This reliability allows each cell to create, on demand, its own suite of purpose-built biological tools. “Proteins are the most sophisticated molecules in the known universe,” Neil King, a biochemist at the University of Washington’s Institute for Protein Design (I.P.D.), told me. In their efficiency, refinement, and subtlety, they surpass pretty much anything that human beings can build.
Today, biochemists engineer proteins to fight infections, produce biofuels, and improve food stability. Usually, they tweak formulas that nature has already discovered, often by evolving new versions of naturally occurring proteins in their labs. But “de novo” protein design—design from scratch—has been “the holy grail of protein science for many decades,” Sarel Fleishman, a biochemist at the Weizmann Institute of Science, in Israel, told me. Designer proteins could help us cure diseases; build new kinds of materials and electronics; clean up the environment; create and transform life itself. In 2018, Frances Arnold, a chemical engineer at the California Institute of Technology, shared the Nobel Prize in Chemistry for her work on protein design. In April, when the coronavirus pandemic was peaking on the coasts, we spoke over video chat. Arnold, framed by palm trees, sat outside her home, in sunny Southern California. I asked how she thought about the potential of protein design. “Well, I think you just have to look at the world behind me, right?” she said. “Nature, for billions of years, has figured out how to extract resources from the environment—sunlight, carbon dioxide—and convert those into remarkable, living, functioning machines. That’s what we want to do—and do it sustainably, right? Do it in a way that life can go on.”
The world is one step closer to having a totally secure internet and an answer to the growing threat of cyber-attacks, thanks to a team of international scientists who have created a unique prototype that could transform how we communicate online.
The invention led by the University of Bristol, revealed today in the journal Science Advances, has the potential to serve millions of users, is understood to be the largest-ever quantum network of its kind, and could be used to secure people’s online communication, particularly in these internet-led times accelerated by the COVID-19 pandemic.

Human limitations are part of the reason we conjured up meta-humans with DNA that enables them to do things we could never dream of doing, such as fly, turn invisible, and regenerate.
The West African lungfish sounds like a creature spawned from science fiction. It can regrow its tail and fins if hungry jaws snap a part of it off, much like a salamander. Its incredible regeneration abilities indicate that these particular traits came from a common vertebrate ancestor — and humans are also vertebrates. Now evolutionary biologist Igor Schneider and his research team are trying to understand the mechanism behind this almost paranormal power, and how it could apply to a human.
The removal of one gene renders poxviruses—a lethal family of viral infections that are known to spread from animals to humans—harmless, a new study in the journal Science Advances reports.
During this ground-breaking study, scientists from the Spanish National Research Council and the University of Surrey investigated the immune response of cells to poxviruses. Poxviruses, such as cowpox and monkeypox, can spread to humans from infected animals, causing skin lesions, fever, swollen lymph nodes and even death.
Viruses contain genetic material which helps them outsmart host cells, enabling replication and the spread of the infection. Cells in the body are comprised of molecules that sense the presence of viruses, sometimes via the recognition of their genetic material, and alert the immune system of an upcoming infection. Poxviruses, unlike other viruses, are highly unusual in that they have large DNA genomes that are replicated exclusively in the cell cytosol, an area of the cell full of sensors. How poxviruses manage to stay undetectable has remained unknown.