Tubular biomarkers linked to sodium avidity in heart failure—may give insights into causes of diuretic resistance. @UCSDCardiology
Tubular biomarkers linked to sodium avidity in heart failure—may give insights into causes of diuretic resistance. @UCSDCardiology
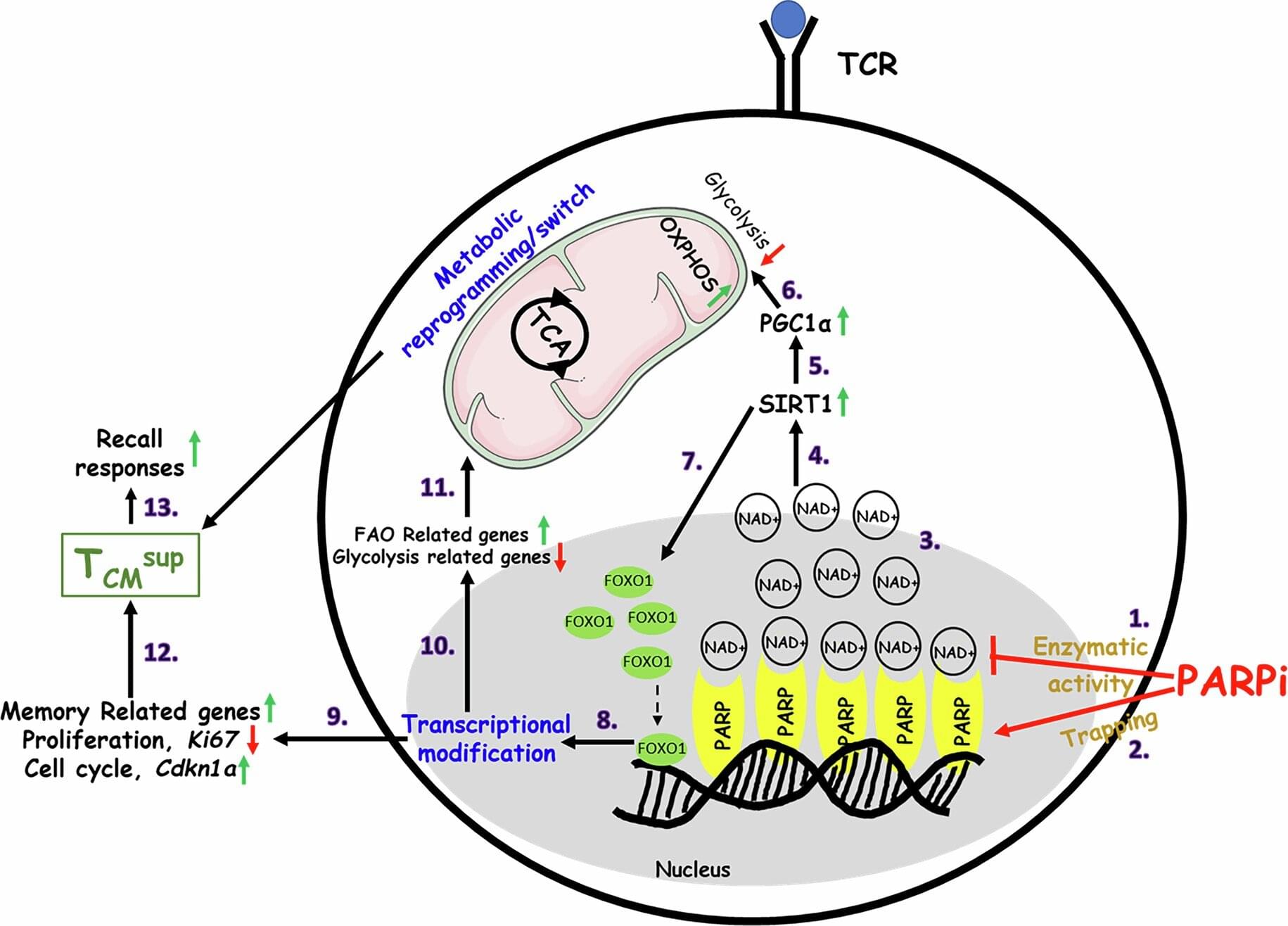
Georgetown University’s Lombardi Comprehensive Cancer Center researchers have identified a new way to reprogram T cells, which are infection and tumor-fighting white blood cells, so that they have a superior memory, thereby making them more effective in killing cancer cells.
The finding, published January 12, 2026, in Nature Immunology, amplifies a known strategy of blocking the cellular activity of PARP, an enzyme that detects DNA abnormalities in cells and repairs them.
“This opens the door to a new area of research in understanding how our immune system works, and as importantly, it opens the way for the development of new strategies for the treatment of cancer,” says Samir N. Khleif, MD, director of The Center for Advanced Immunotherapy Research and the director of Loop Immuno-Oncology Research Laboratory at Georgetown’s Lombardi.

The devastating illness deteriorates your brain’s ability to think, remember things and can even alter your behaviour.
While some studies have discovered that engaging in a pretty gross habit or reaching a daily step count can reduce the risk of developing Alzheimer’s disease (AD), for over a century, scientists have considered it an irreversible illness. This is why research has focused on preventing or slowing its progression, rather than recovery.
However, a new study challenges this long-held belief by testing whether brains already severely afflicted with advanced AD could recover.

Inside the body, a 24-hour rhythm, known as the circadian rhythm, quietly coordinates when we sleep, wake, eat, and recover. This internal timing system helps keep organs and hormones working in sync.
When it becomes disrupted, the effects may extend well beyond poor sleep, with growing evidence suggesting consequences for long-term brain health.
A large 2025 study of more than 2,000 people with an average age of 79 found that those with a strong circadian rhythm had an almost halved risk of developing dementia. Circadian rhythms regulate daily processes, including sleep timing, hormone release, heart rate, and body temperature.
Further Reading.
This ‘digital brain’ could soon simulate ethically forbidden experiments.
https://ebrains.eu/news-and-events/2025/ten-years-of-pd14-mi…i-research.
A foundation model to predict and capture human cognition.
https://www.nature.com/articles/s41586-025-09215-4
First totally synthetic human brain model has been realized.
https://newatlas.com/medical/synthetic-human-brain-models/
#science #news #explained #research #sciencenews #biotech #robots #ai #artificialintelligence #organoid
Previously, we described that Adenine, Thymine, Cytosine, and Guanine nucleobases were superconductors in a quantum superposition of phases on each side of the central hydrogen bond acting as a Josephson Junction. Genomic DNA has two strands wrapped helically around one another, but during transcription, they are separated by the RNA polymerase II to form a molecular condensate called the transcription bubble. Successive steps involve the bubble translocation along the gene body. This work aims to modulate DNA as a combination of n-nonperturbative circuits quantum electrodynamics with nine Radio-Frequency Superconducting Quantum Interference Devices (SQUIDs) inside. A bus can be coupled capacitively to a single-mode microwave resonator. The cavity mode and the bus can mediate long-range, fast interaction between neighboring and distant DNA SQUID qubits.
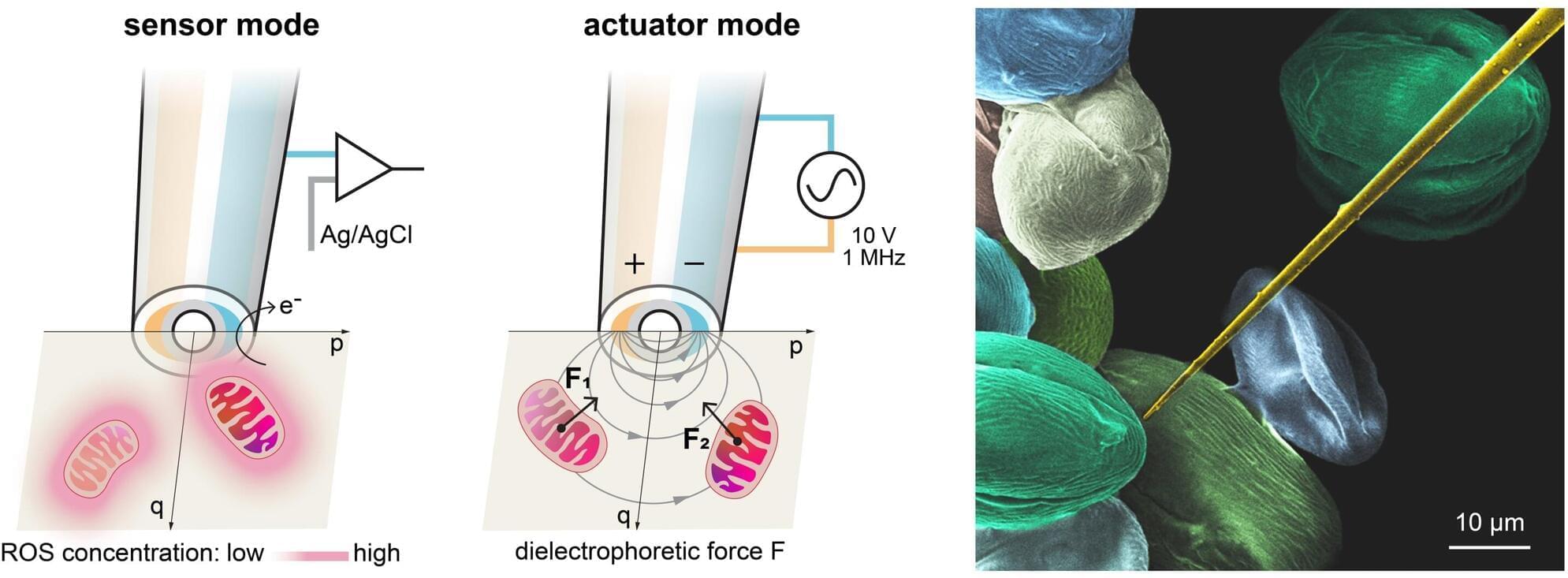
Mitochondrial dysfunction is associated with various chronic diseases and cancers, including neurodegenerative diseases and metabolic syndrome. Gently extracting a single mitochondrion from within a living cell—without causing damage and without the guidance of fluorescent makers—has long been a challenge akin to threading a needle in a storm for scientists.
A team led by Prof. Richard Gu Hongri, Assistant Professor in the Division of Integrative Systems and Design of the Academy of Interdisciplinary Studies at The Hong Kong University of Science and Technology (HKUST), in collaboration with experts in mechanical engineering and biomedicine, has developed an automated robotic nanoprobe.
The device can navigate within a living cell, sense metabolic whispers in real time, and pluck an individual mitochondrion for analysis or—all without the need for fluorescent labeling. It is the world’s first cell-manipulation nanoprobe that integrates both sensors and actuators at its tip, enabling a micro-robot to autonomously navigate inside live cells. The breakthrough holds great promise for advancing future treatment strategies for chronic diseases and cancer.
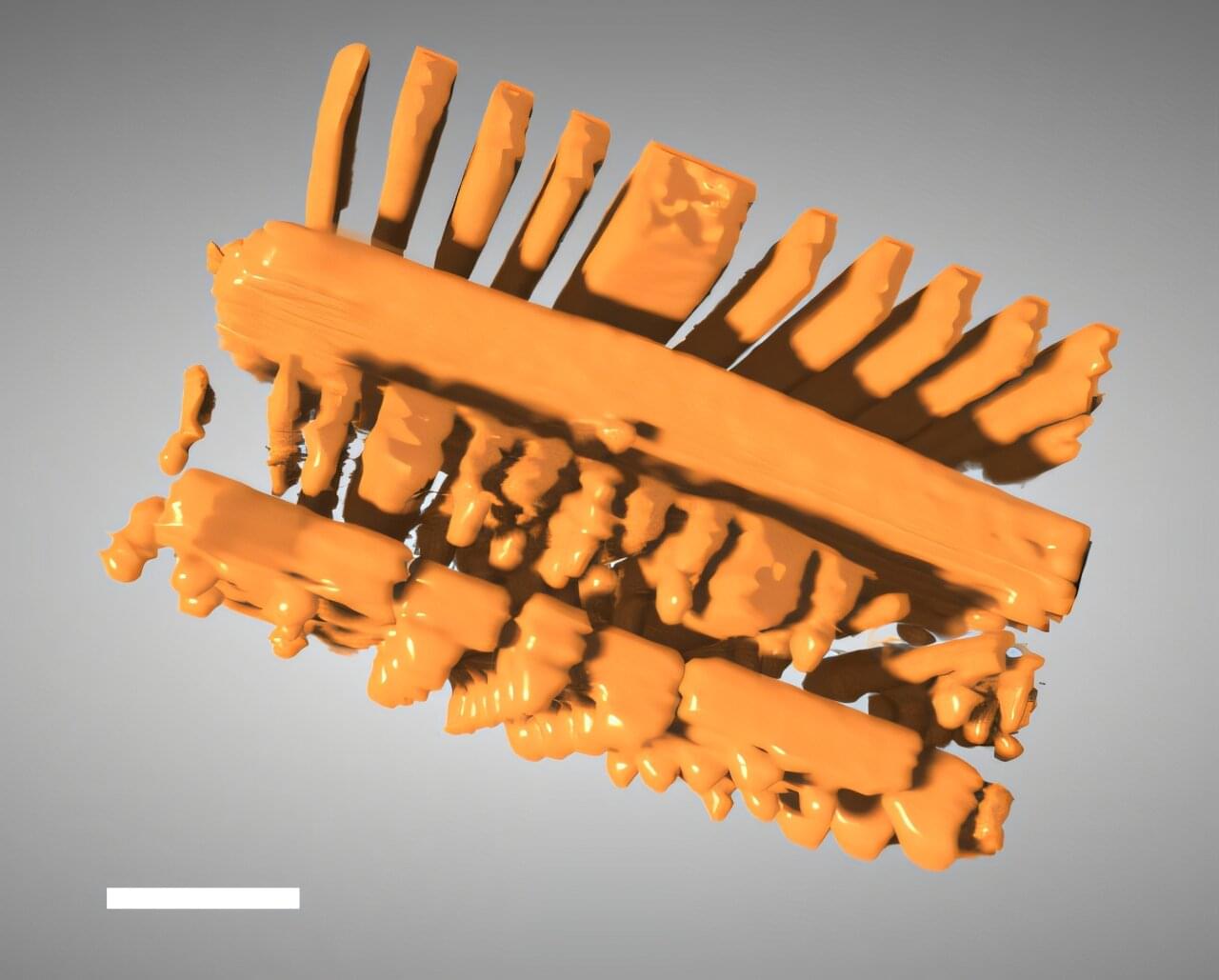
X-ray tomography is a powerful tool that enables scientists and engineers to peer inside of objects in 3D, including computer chips and advanced battery materials, without performing anything invasive. It’s the same basic method behind medical CT scans.
Scientists or technicians capture X-ray images as an object is rotated, and then advanced software mathematically reconstructs the object’s 3D internal structure. But imaging fine details on the nanoscale, like features on a microchip, requires a much higher spatial resolution than a typical medical CT scan—about 10,000 times higher.
The Hard X-ray Nanoprobe (HXN) beamline at the National Synchrotron Light Source II (NSLS-II), a U.S. Department of Energy (DOE) Office of Science user facility at DOE’s Brookhaven National Laboratory, is able to achieve that kind of resolution with X-rays that are more than a billion times brighter than traditional CT scans.
Artificial intelligence (AI) is increasingly used to analyze medical images, materials data and scientific measurements, but many systems struggle when real-world data do not match ideal conditions. Measurements collected from different instruments, experiments or simulations often vary widely in resolution, noise and reliability. Traditional machine-learning models typically assume those differences are negligible—an assumption that can limit accuracy and trustworthiness.
To address this issue, Penn State researchers have developed a new artificial intelligence framework with potential implications for fields ranging from Alzheimer’s disease research to advanced materials design. The approach, called ZENN and detailed in a study that was featured as a showcase in the Proceedings of the National Academy of Sciences, teaches AI models to recognize and adapt to hidden differences in data quality rather than ignoring them.
ZENN, short for Zentropy-Embedded Neural Networks, was developed by Shun Wang, postdoctoral scholar of materials science and engineering; Wenrui Hao, professor of mathematics, Zi-Kui Liu, professor of materials science and engineering, and Shunli Shang, research professor of materials science and engineering.
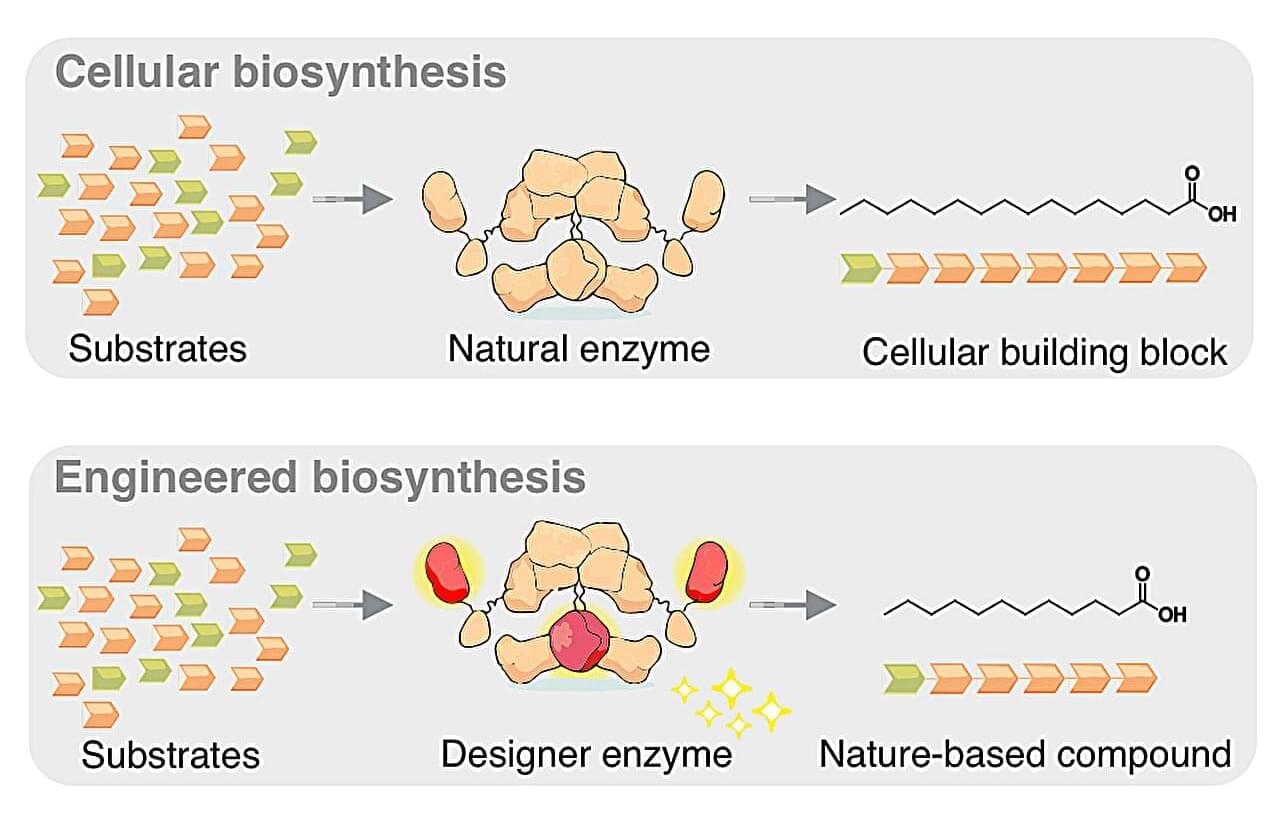
Whether they are laundry detergents, mascara, or Christmas chocolate, many everyday products contain fatty acids from palm oil or coconut oil. However, the extraction of these raw materials is associated with massive environmental issues: Rainforests are cleared, habitats for endangered species are destroyed, and traditional farmers lose their livelihoods.
A research team led by Prof. Martin Grininger at Goethe University in Frankfurt, Germany, has now developed a biotechnological approach that could enable a more environmentally friendly production method. The team’s work appears in Nature Chemical Biology.