This led to the discovery that myelin swellings have a dynamic character: they can not only grow, but also shrink and even recover completely. It also turns out that the activity of the underlying nerve fibre plays an important role; more activity of the nerve fibre leads to more and bigger swellings, while less activity allows for possible recovery.
The authors show that in human multiple sclerosis tissue, myelin swelling is also dynamic and is prominent around active lesions. Science Mission sciencenewshighlights.
An international research team have gained new insights into the dynamics of myelin swellings in the brain. Myelin swellings are considered as the precursor of lesions in the brain of people with multiple sclerosis (MS). The results have been recently published in the leading magazine Science.
MS is characterised by lesions in the brain and the spinal cord. Aside from these inflammations, damage can also be visible in the myelin; the protective layer surrounding nerve fibers. Myelin swellings are seen as a precursor for damaged myelin.
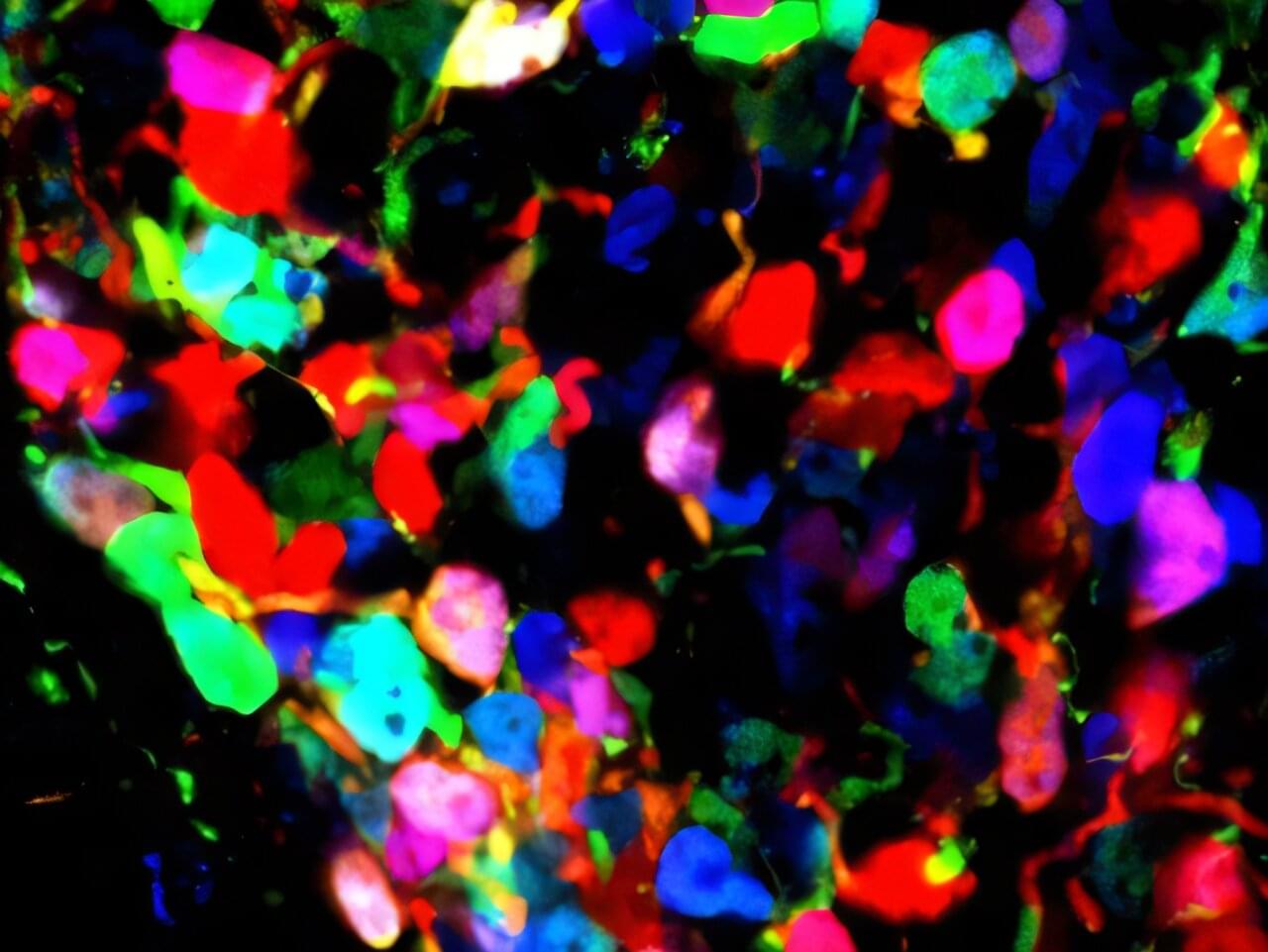
The research team used advanced microscopy techniques and different models – from zebrafish and mouse models to human brain tissue – to research the formation of this damage.