It’s a fact of life: Some people age better than others. Some ease into their 90s with mind and body intact, while others battle diabetes, Alzheimer’s or mobility issues decades earlier. Some can withstand a bad fall or bout of the flu with ease, while others never leave the hospital again.
New University of Colorado Boulder-led research, published in Nature Genetics, sheds light on why that is.
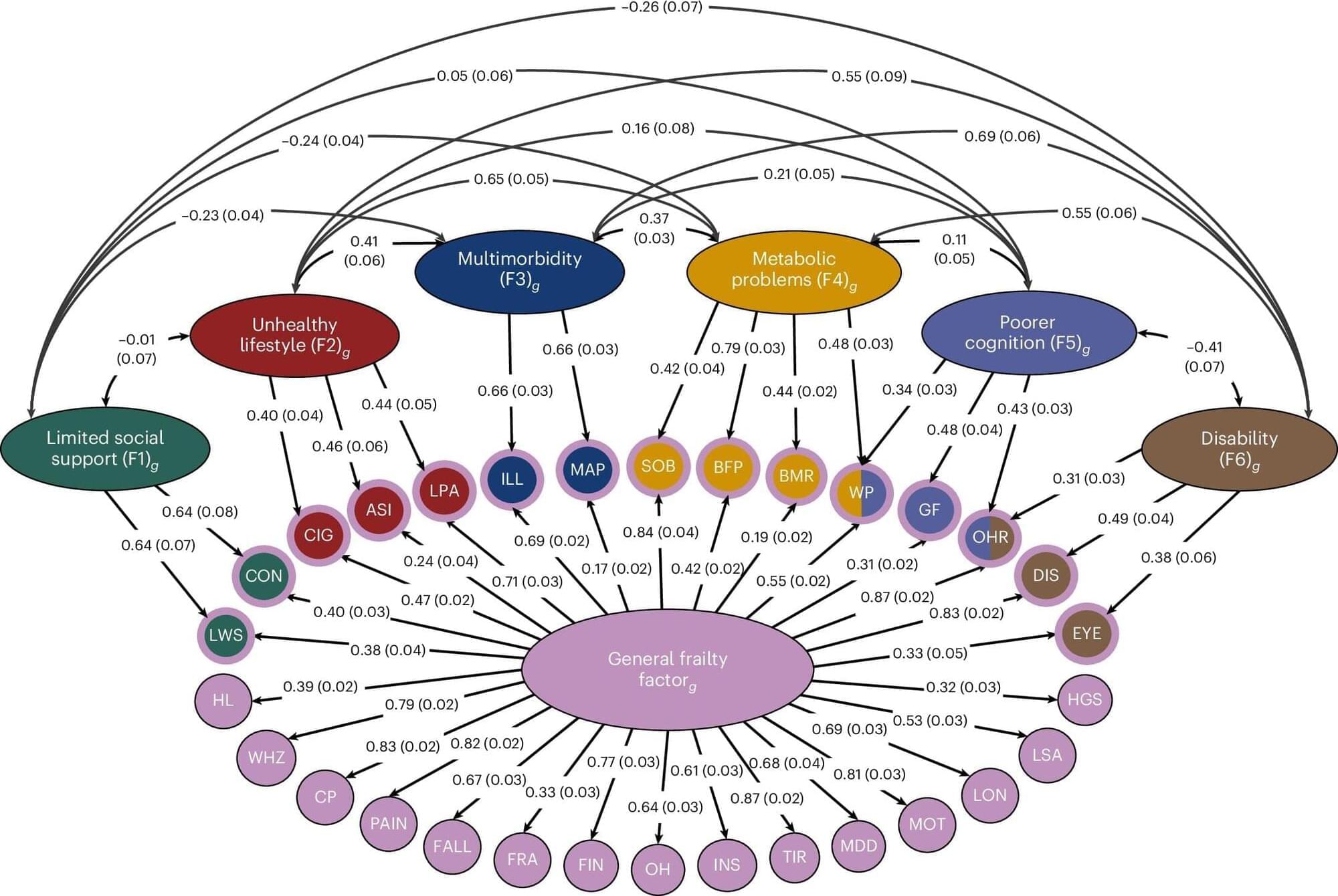
In it, an international team of co-authors identifies more than 400 genes associated with accelerated aging across seven different sub-types. The study reveals that different groups of genes underlie different kinds of disordered aging, a.k.a. frailty, ranging from cognitive decline to mobility issues to social isolation.