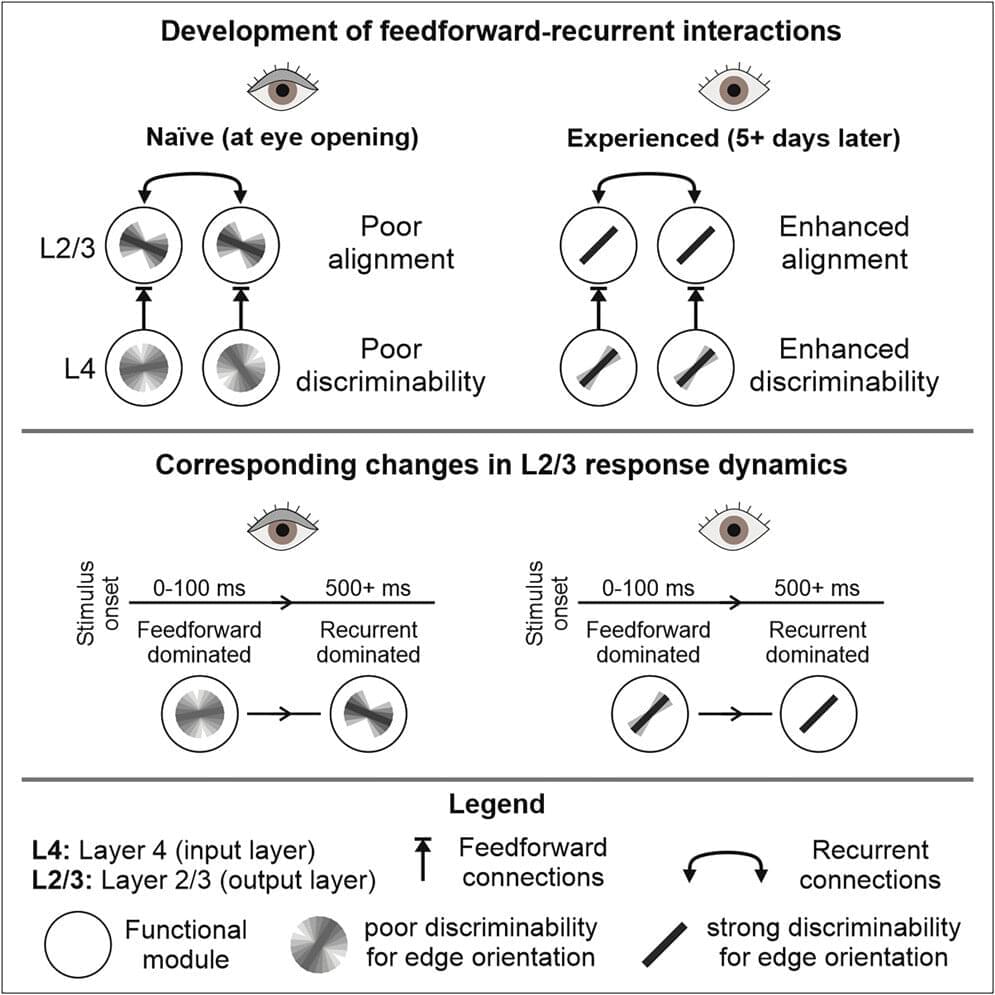
We take our understanding of where we are for granted, until we lose it. When we get lost in nature or a new city, our eyes and brains kick into gear, seeking familiar objects that tell us where we are.
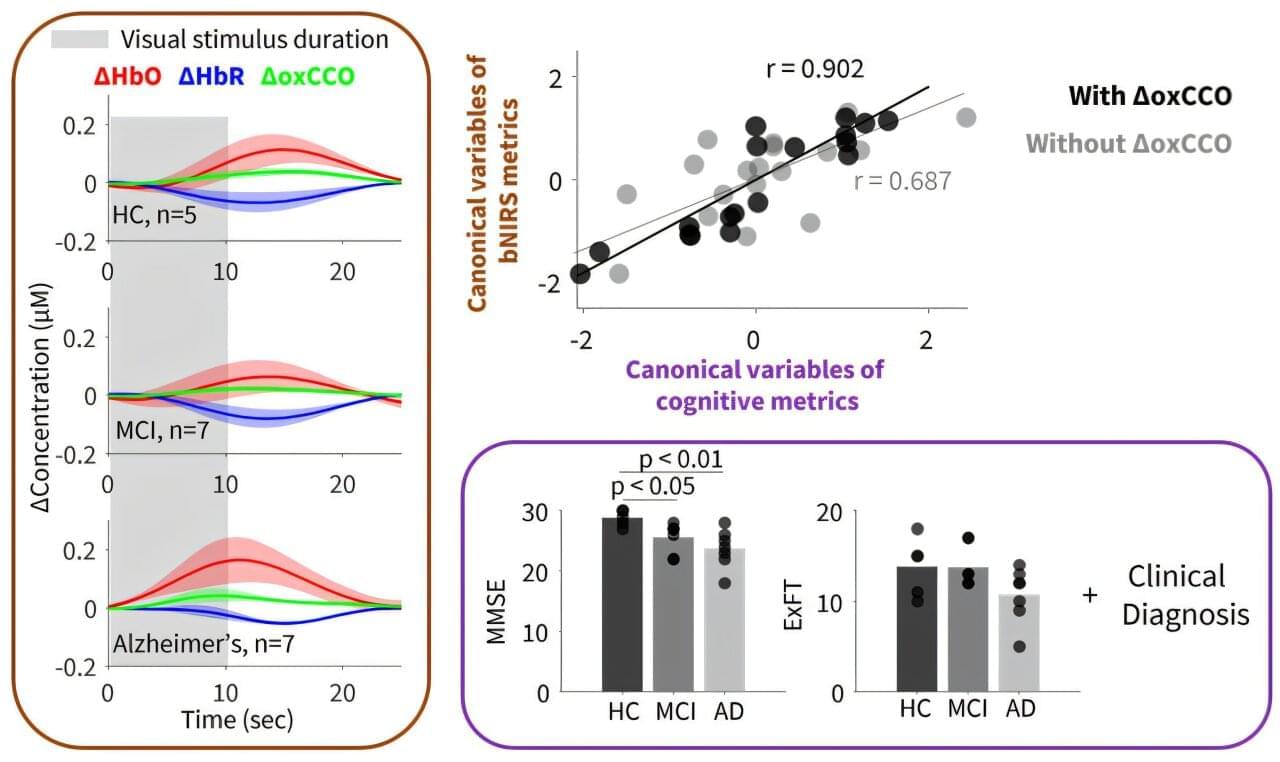
How our brains distinguish objects from background when finding direction, however, was largely a mystery. A new study provides valuable insight into this process, with possible implications for disorientation-causing conditions such as Alzheimer’s. The work is published in the journal Science.
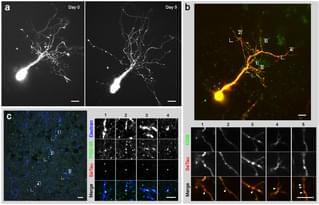
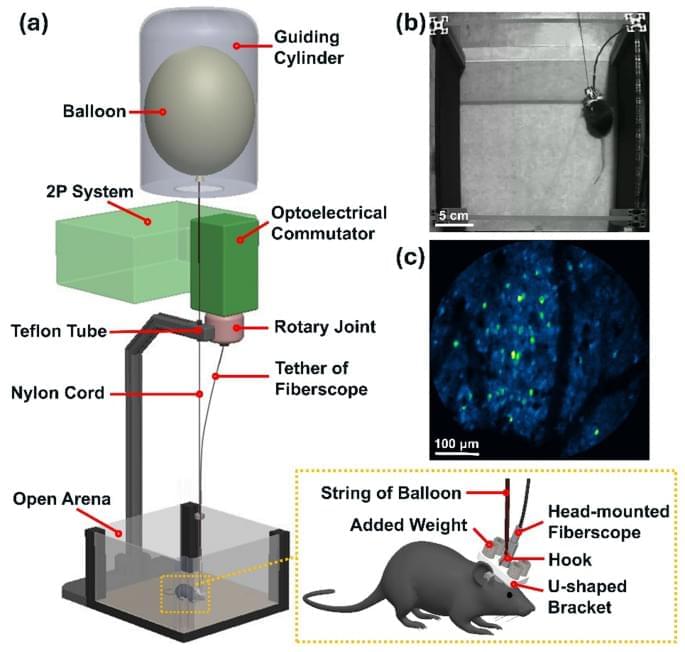
The scientists, based at The Neuro (Montreal Neurological Institute-Hospital) of McGill University and the University Medical Center Göttingen, ran an experiment with mice using ultrasound imaging to measure and record brain activity. The mice were shown visual stimuli, either an object or a scrambled image showing no distinct object.