How 6 small molecules made old human cells act young again. No gene editing, no stem cells. Just science.


Researchers publishing in Aging Cell have used single-cell transcriptomics to discover new insights into how neural stem cells (NSCs) change with aging.
Adults do generate neurons
The adult brain does generate new neurons [1], particularly in the hippocampus, the part of the brain responsible for memory formation [2]. Neurogenesis is limited to very specific niches, however, and does not occur across the entire brain [3]. This is accomplished by NSCs, cells that can differentiate into neural progenitors (NPs), which can themselves differentiate into both neurons and astrocytes and have less ability to proliferate [4]. Astrocytes are helper cells that support neurons’ connections and metabolism [5].
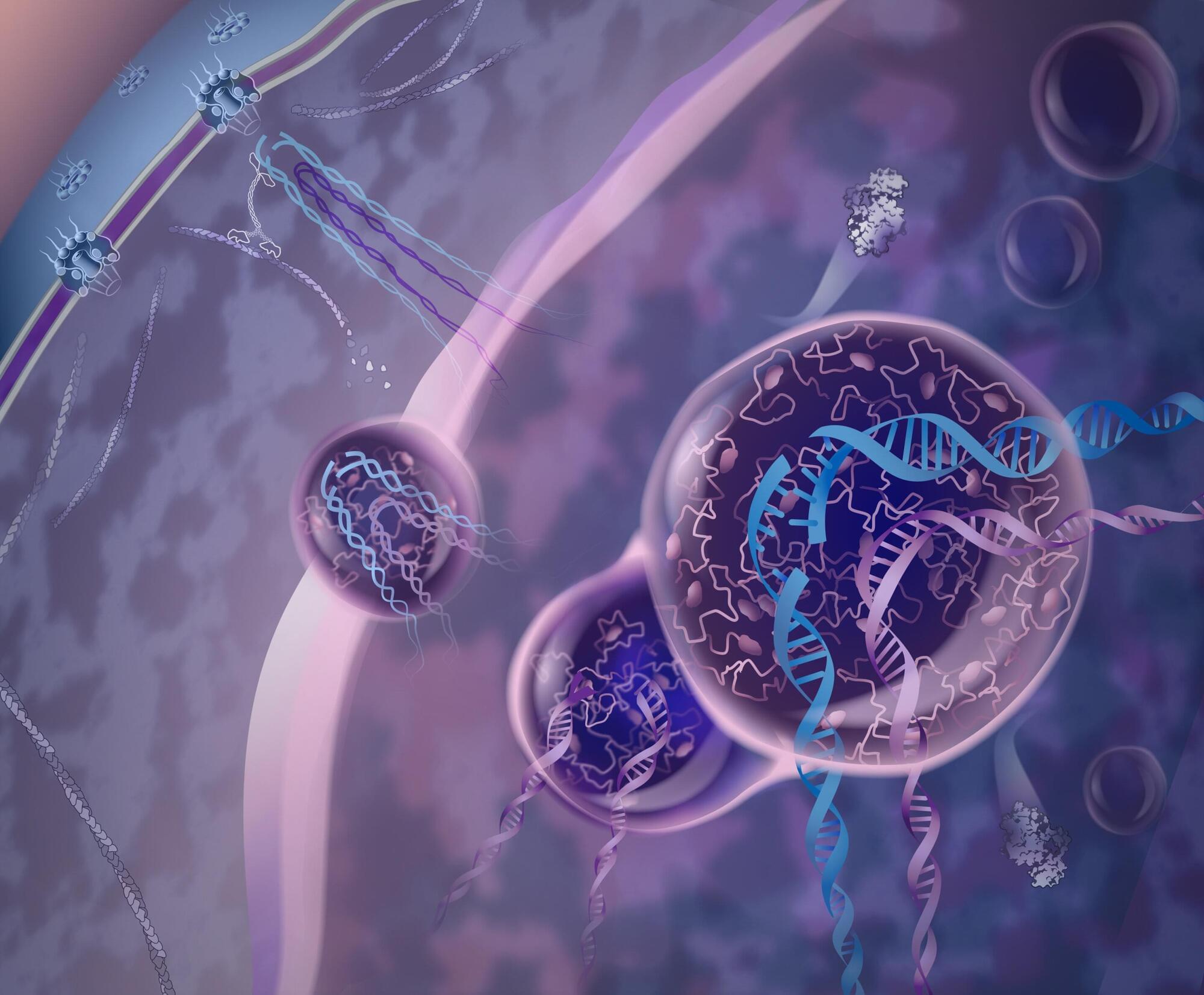
When DNA breaks inside the cell, it can spell disaster, especially if the damage occurs in areas of the genome that are difficult to repair. Now, scientists Irene Chiolo and Chiara Merigliano at the USC Dornsife College of Letters, Arts and Sciences have discovered that a protein called Nup98, long known for helping traffic molecules in and out of the cell’s nucleus, plays another surprising role: guiding the cell’s most delicate repairs and reducing the risk of genetic mistakes that can lead to cancer. Their findings were published in Molecular Cell.
With support from the National Institutes of Health, the National Science Foundation, and the American Cancer Society, the researchers revealed that Nup98 forms droplet-like structures deep inside the nucleus. These “condensates” act as protective bubbles around broken strands of DNA in areas called heterochromatin—zones where the genetic material is so tightly packed that making accurate repairs is especially challenging.
Heterochromatin—a major focus of Chiolo’s research—is filled with repeated DNA sequences, making it easy for the cell to confuse one stretch for another. Nup98’s droplets help lift the damaged section out of that dense zone and create a safer space where it can be repaired accurately, reducing the chance of genetic mix-ups that could lead to cancer.
In this TEDx talk, Dante Muratore shows the transformative potential of brain-computer interfaces. He explains how they can be used to help patients suffering from neurodegenerative diseases, focusing on an artificial retina he and his team are developing to cure blindness in patients with macular degeneration and retinitis pigmentosa. He also describes how brain-computer interfaces will change what it means to be human in the future and challenges us to think deeply about the use we want to make of this technology in society.
Professor of Bioelectronics at Delft University of Technology, where he leads the Smart Brain Interfaces group. His research group explores hardware and system solutions for brain-computer interfaces capable of interacting with the nervous system. The group is working, in collaboration with leading universities in the field, on a microchip to be implanted in the retina to improve the lives of people affected by retinitis pigmentosa and degenerative maculopathy.
This talk was given at a TEDx event using the TED conference format but independently organized by a local community.

Artificial intelligence (A.I.) has recently become a buzzword in so many aspects of our lives, but it has been used to some degree in health care for a while. One area of health care where A.I. has made significant strides is the diagnosis and treatment of prostate cancer.
“We are just at the tip of the iceberg of utilizing A.I. for prostate cancer,” says Dr. David D. Yang, a radiation oncologist with Harvard-affiliated Brigham and Women’s Hospital and Dana-Farber Cancer Institute. “So far, it has been shown to help improve the care for men with prostate cancer in limited, yet effective ways.”
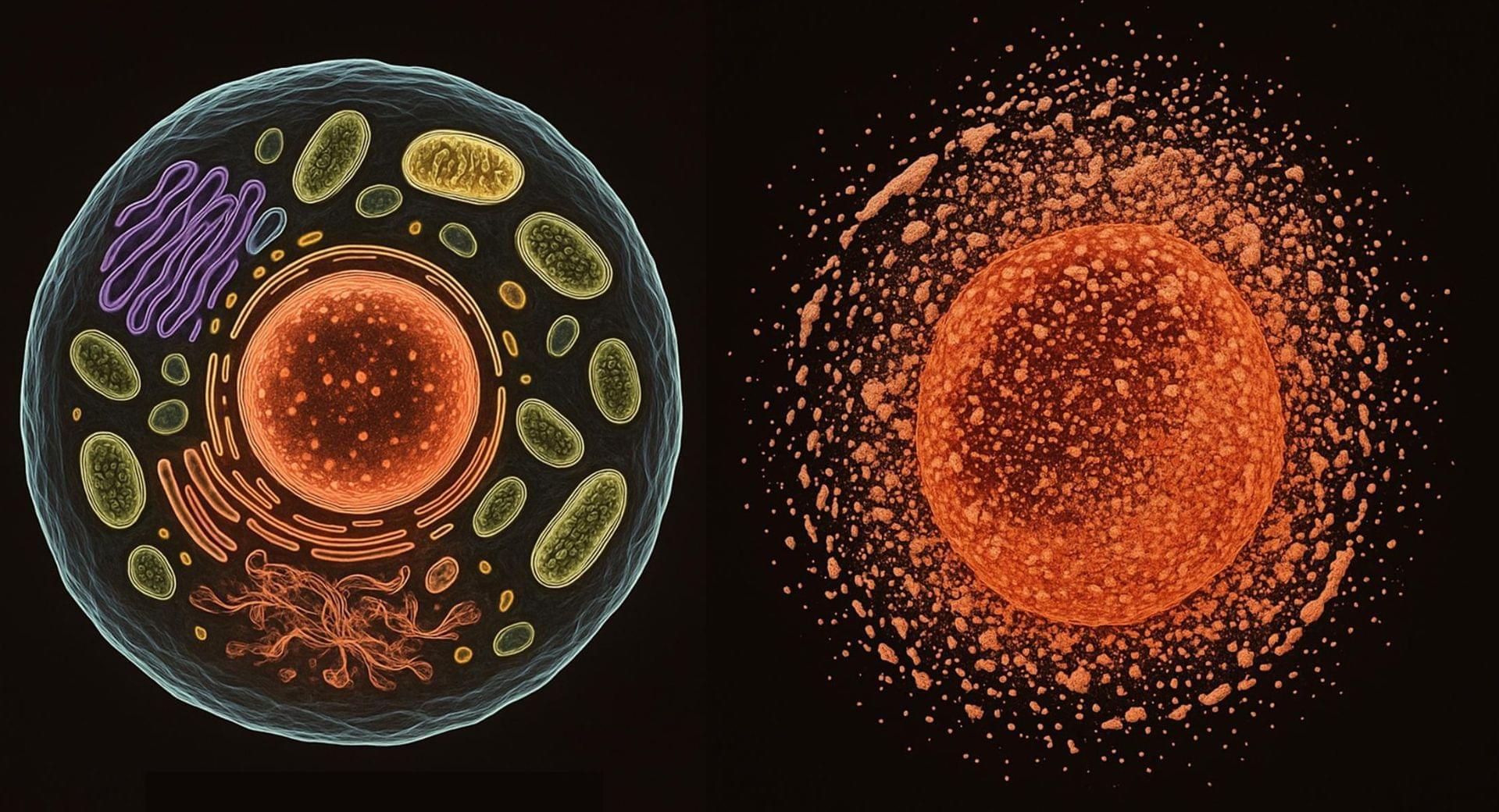
Dr Keith Siew, one of the study authors, says, “Nobody really likes talking about death, even cell death, which is perhaps why the physiology of death is so poorly understood. And in a way necrosis is death. If enough cells die, then tissues die, then we die. The question is what would happen if we could pause or stop necrosis.”
“Necrosis remains one of the last frontiers in medicine – a common thread across aging, disease, space biology, and scientific progress itself,” adds Dr Carina Kern, lead author of the study.
Necrosis occurs when cells are overwhelmed by injury, infection, or stress. The process floods cells with calcium, disrupting vital functions and causing the cell to rupture. This sudden collapse spills toxic molecules into surrounding tissue, triggering inflammation and accelerating damage.
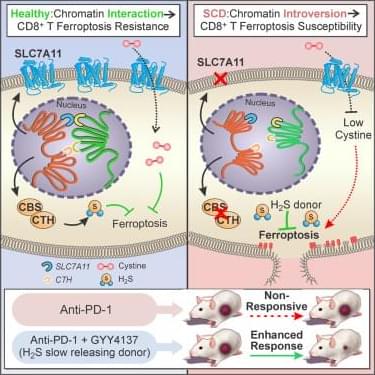
How sickle cell disease suppresses antitumor immunity.
Sickle cell disease (SCD) have a higher risk of developing certain cancers than the general population, but the mechanisms driving this increased risk remain unclear.
SCD inhibits CD8+ T cell function in the tumor microenvironment, potentially affecting cancer immunotherapy.
The researchers reveal that SCD alters the 3D genome architecture of CD8+ T cells, triggering ferroptosis and impairing antitumor response resulting in reduced expression of anti-ferroptotic genes, including SLC7A11 and hydrogen sulfide (H2S) biogenesis genes, thereby increasing susceptibility to ferroptosis.
They also demonstrate that hydrogen sulfide treatment rescued SLC7A11 expression, mitigated ferroptosis and enhanced immune and anti-tumor responses, thereby offering new avenues for precision immunotherapy in patients with inherited disorders. https://sciencemission.com/Sickle-cell-disease
Sickle cell disease (SCD) inhibits CD8+ T cell function in the tumor microenvironment, potentially affecting cancer immunotherapy. Zhao, Hu, Deng, et al. reveal that SCD alters the 3D genome architecture of CD8+ T cells, triggering ferroptosis and impairing anti-tumor responses, which can be reversed by hydrogen sulfide treatment, offering new avenues for precision immunotherapy in patients with inherited disorders.

A new study published in JAMA Psychiatry makes the case that symptom provocation may significantly improve the clinical effectiveness of repetitive transcranial magnetic stimulation (rTMS), a noninvasive brain stimulation method used to treat depression, obsessive-compulsive disorder (OCD) and nicotine dependence.
The study was conceptualized, designed and supervised by Heather Burrell Ward, MD, assistant professor of Psychiatry and Behavioral Sciences and director of Neuromodulation Research, in collaboration with Simon Vandekar, Ph.D., associate professor of Biostatistics and Daniel Bello and Megan Jones, two students in their respective labs.
This is the first large-scale meta-analysis to examine whether deliberately triggering symptoms immediately before administering rTMS enhances treatment outcomes.
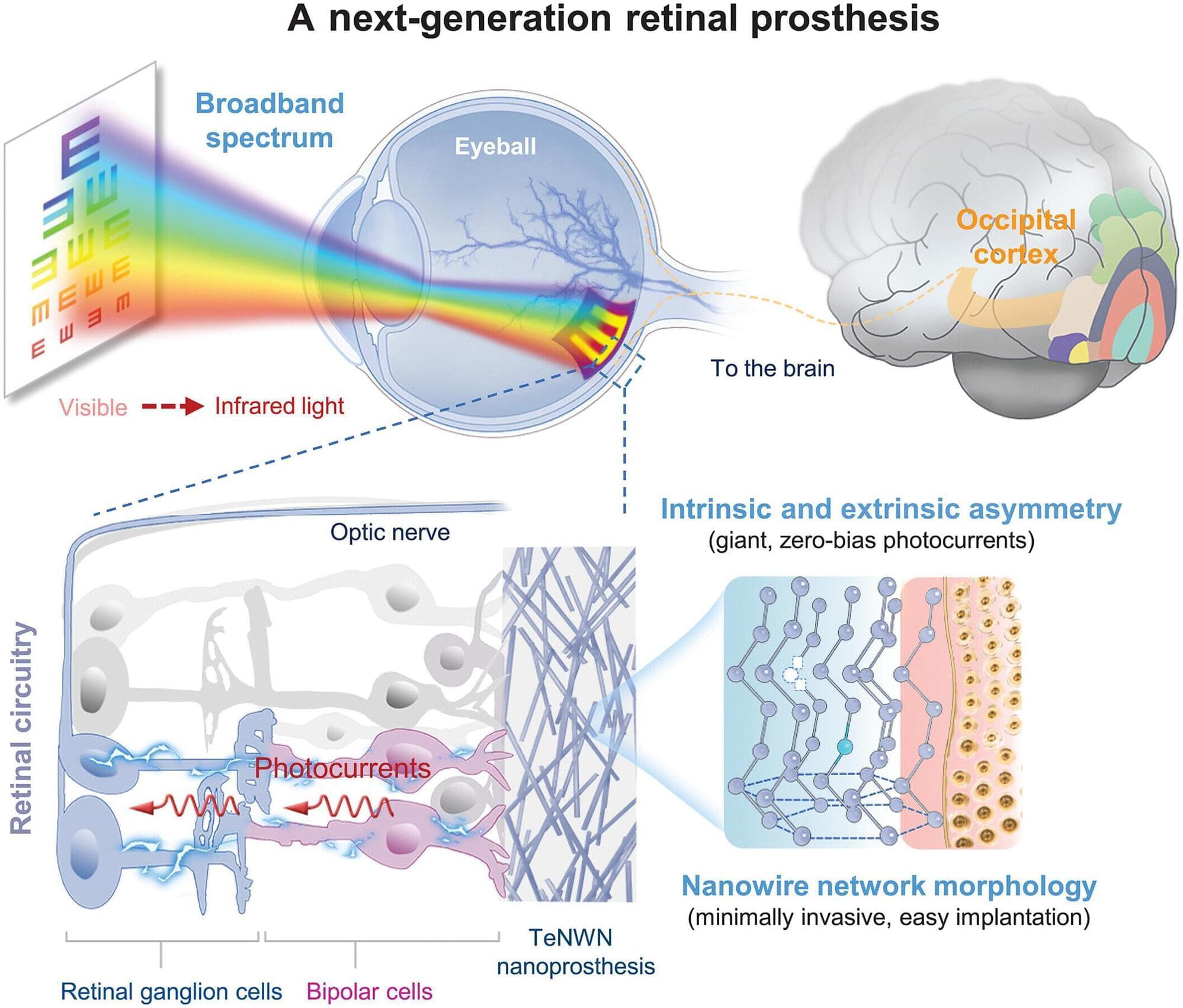
A team from Fudan University, the Shanghai Institute of Technical Physics, the Beijing University of Posts and Telecommunications and Shaoxin Laboratory, all in China, has developed a retinal prosthesis woven from metal nanowires that partially restored vision in blind mice.
In their paper published in the journal Science, the group describes how they created tellurium nanowires and interlaced them to create a retinal prosthesis. Eduardo Fernández, with University Miguel Hernández, in Spain, has published a Perspective piece in the same journal issue outlining the work done by the team on this new effort.
Finding a way to cure blindness has been a major goal for scientists for many years, and such efforts have paid off for some types of blindness, such as those caused by cataracts. Other types of blindness associated with damage to the retina, however, have proven too difficult to overcome in most cases. For this research, the team in China tried a new approach to treating such types of blindness by building a mesh out of a semiconductor and affixing it to the back of the eye, where it could send signals to the optic nerve.
