A new study reveals that bacteria can survive antibiotic treatment through two fundamentally different “shutdown modes,” not just the classic idea of dormancy. The paper is published in the journal Science Advances.
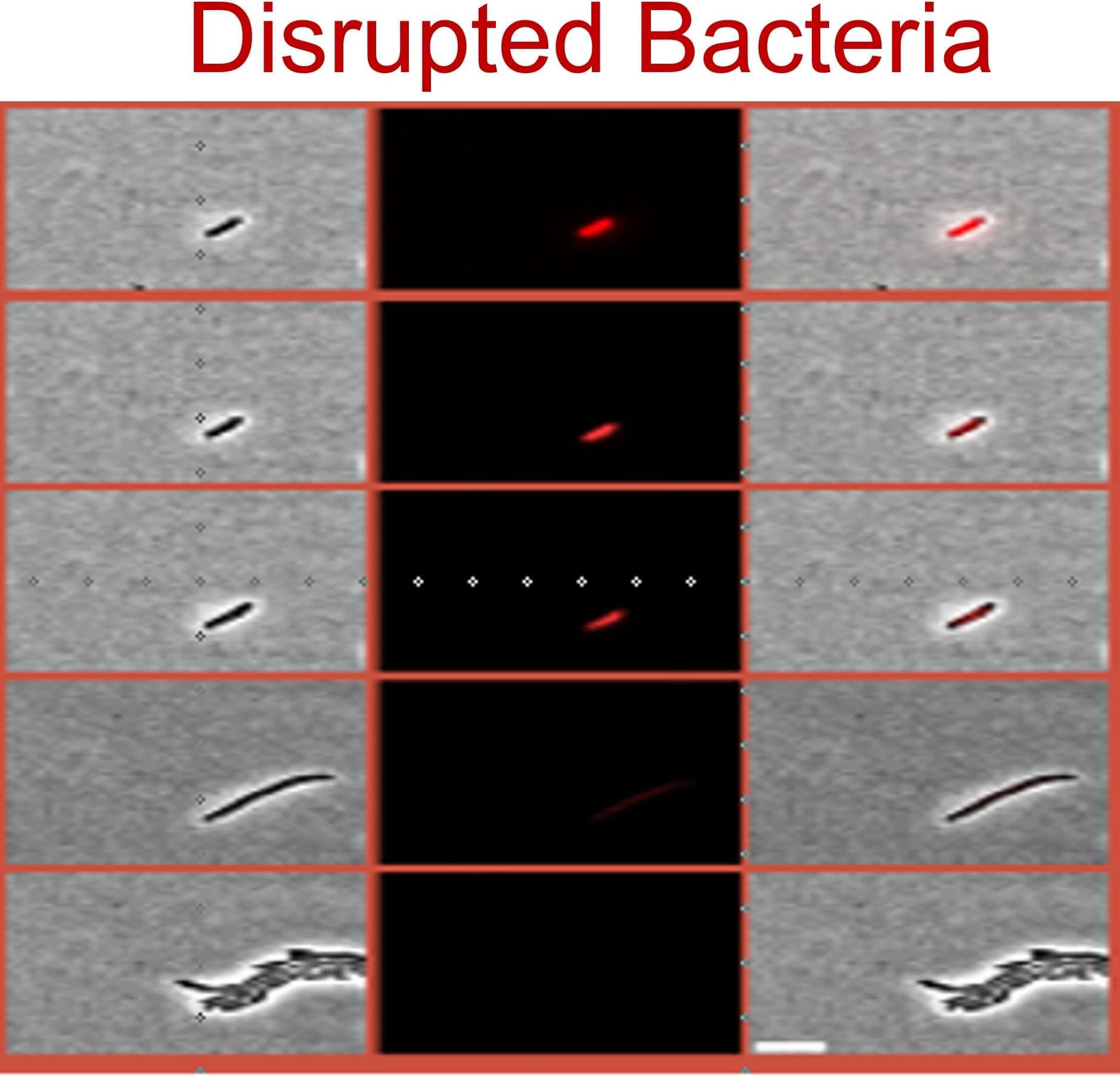
The researchers show that some cells enter a regulated, protective growth arrest, a controlled dormant state that shields them from antibiotics, while others survive in a disrupted, dysregulated growth arrest, a malfunctioning state marked by vulnerabilities, especially impaired cell membrane stability. This distinction is important because antibiotic persistence is a major cause of treatment failure and relapsing infections even when bacteria are not genetically resistant, and it has remained scientifically confusing for years, with studies reporting conflicting results.
By demonstrating that persistence can come from two distinct biological states, the work helps explain those contradictions and provides a practical path forward: different persister types may require different treatment strategies, making it possible to design more effective therapies that prevent infections from coming back.