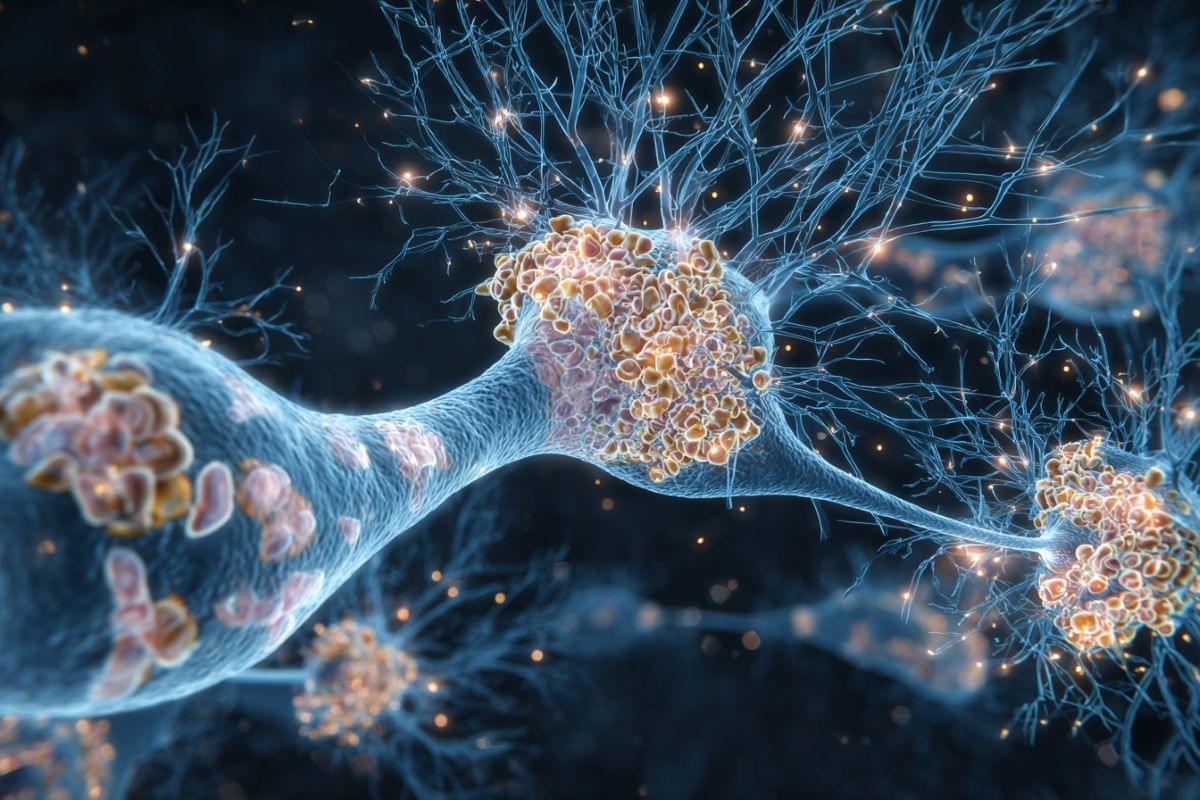
For decades now, the commonly-accepted view among neuroscientists has been that following amputation of a limb, neighboring regions rearrange and essentially take over the area previously assigned to the now missing limb. This has relied on evidence from studies carried out after amputation, without comparing activity in the brain maps beforehand.
To investigate this contradiction, a team of researchers followed three individuals due to undergo amputation of one of their hands. This is the first time a study has looked at the hand and face maps of individuals both before and after amputation.
The researchers examined the signals from the pre-amputation finger maps and compared them against the maps post-amputation. Analysis of the ‘before’ and ‘after’ images revealed a remarkable consistency: even with their hand now missing, the corresponding brain region activated in an almost identical manner.
The study’s senior author, said: Because of our previous work, we suspected that the brain maps would be largely unchanged, but the extent to which the map of the missing limb remained intact was jaw-dropping.
To complement their findings, the researchers compared their case studies to 26 participants who had had upper limbs amputated, on average 23.5 years beforehand. These individuals showed similar brain representations of the hand and lips to those in their three case studies, suggesting long-term evidence for the stability of hand and lip representations despite amputation.
The brain holds a ‘map’ of the body that remains unchanged even after a limb has been amputated, contrary to the prevailing view that it rearranges itself to compensate for the loss, according to new research.