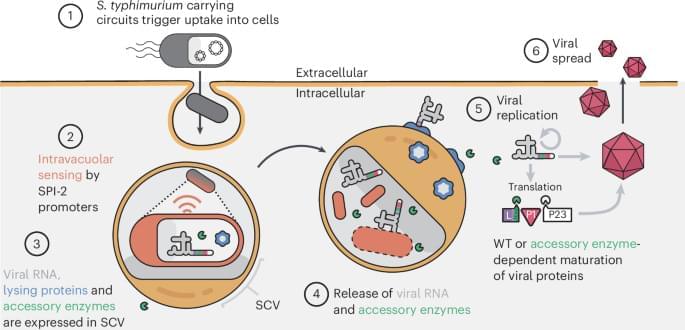
CAPPSID relies on an engineered S. typhimurium to act as a synthetic ‘capsid’ to transcribe and deliver viral RNA inside cancer cells, launching a virus that can directly lyse surrounding cells.

A Northwestern Medicine study has uncovered new insights that may aid in understanding and potentially treating one of the most common and aggressive forms of non-Hodgkin lymphoma, according to findings published in Science Advances.
The study described critical differences in B-cell receptor (BCR) types that may influence the progression and treatment of diffuse large B-cell lymphoma and other forms of B-cell leukemia and lymphomas, which affect more than 80,000 Americans each year.
“B-cells, which are responsible for producing antibodies, rely on BCRs for survival and growth. While most research has focused on the IgM variant of BCRs, this study sheds light on the lesser-understood IgG1 variant,” said Vipul Shukla, Ph.D., assistant professor of Cell and Developmental Biology, who was co-senior author of the study.
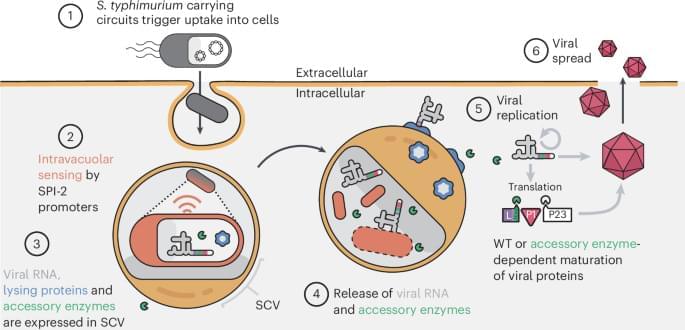
In the U.S., one in five of the 37 million adults who has diabetes doesn’t know it. Current methods of diagnosing diabetes and prediabetes usually require a visit to a doctor’s office or lab work, both of which can be expensive and time-consuming. Now, diagnosing diabetes and prediabetes may be as simple as breathing.
A research team led by Huanyu “Larry” Cheng, James L. Henderson, Jr. Memorial Associate Professor of Engineering Science and Mechanics at Penn State, has developed a sensor that can help diagnose diabetes and prediabetes on-site in a few minutes using just a breath sample. Their results are published in the Chemical Engineering Journal.
Previous diagnostic methods often used glucose found in blood or sweat, but this sensor detects acetone levels in the breath. While everyone’s breath contains acetone as a byproduct of burning fat, acetone levels above a threshold of about 1.8 parts per million indicate diabetes.

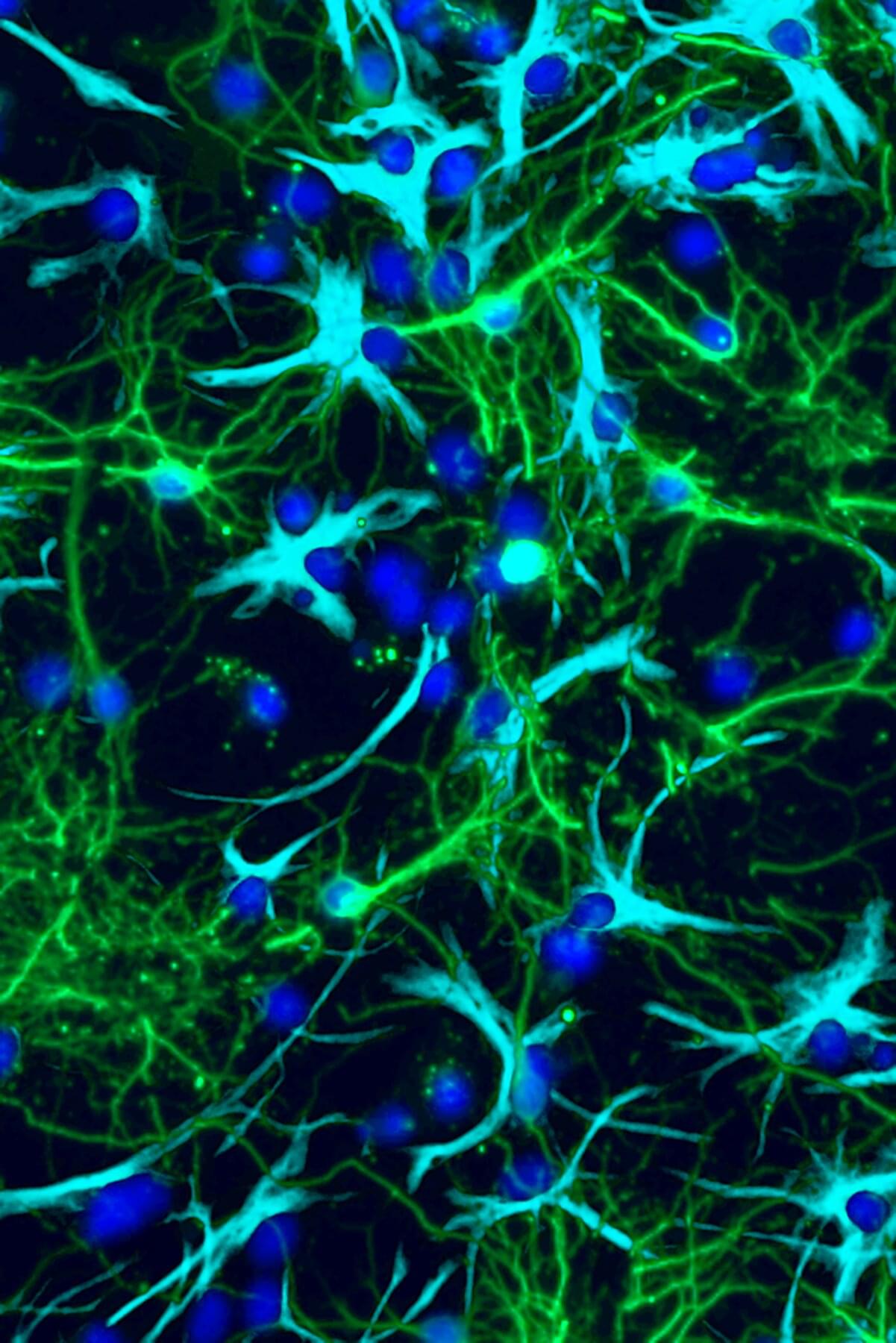
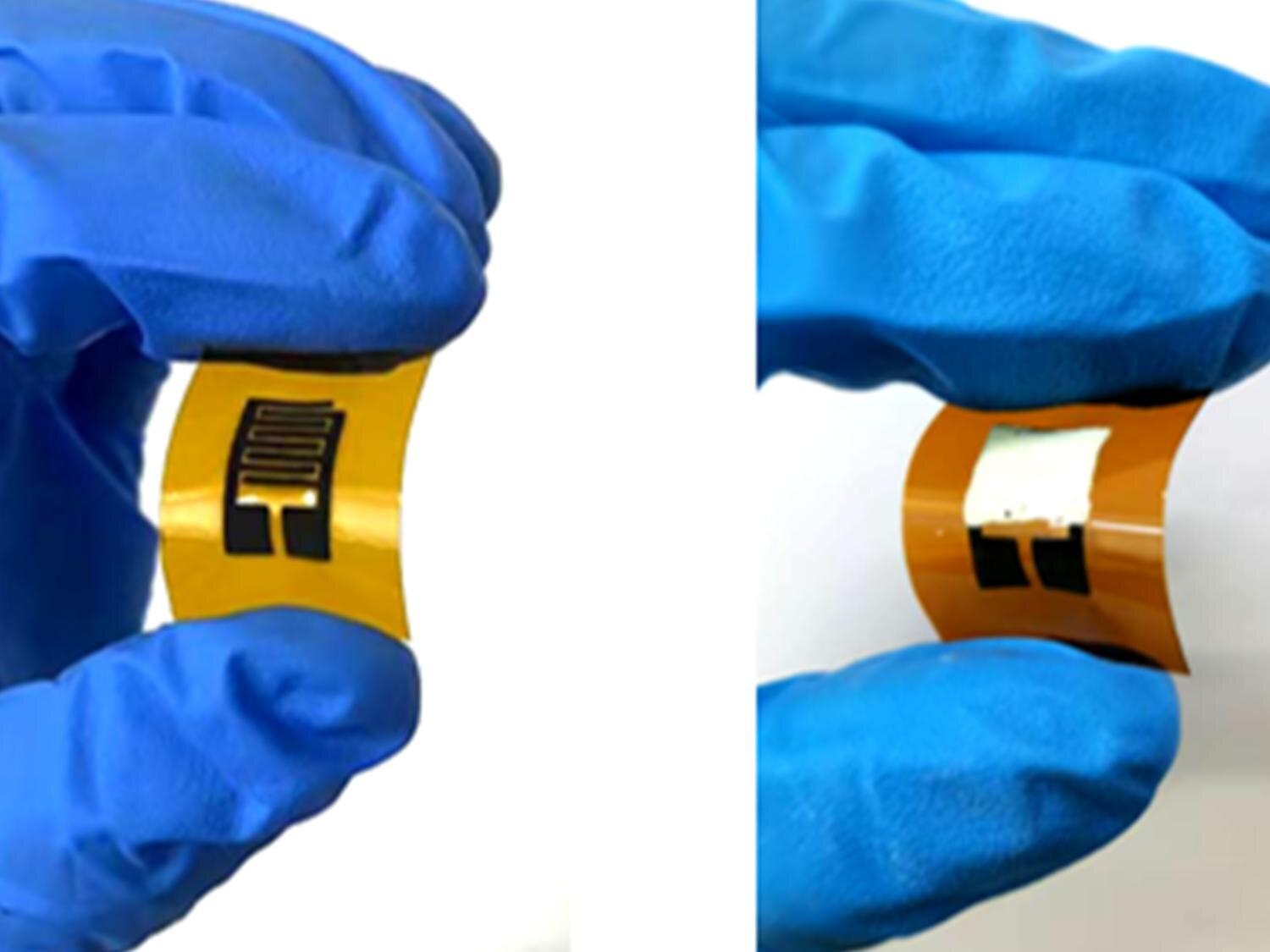
The most common type of brain tumor in children, pilocytic astrocytoma (PA), accounts for about 15% of all pediatric brain tumors. Although this type of tumor is usually not life-threatening, the unchecked growth of tumor cells can disrupt normal brain development and function.
Current treatments focus mainly on removing the tumor cells, but recent studies have shown that non-cancerous cells, such as nerve cells, also play a role in brain tumor formation and growth, suggesting novel approaches to treating these cancers.
Scientists have long known that a nerve cell signaling chemical called glutamate can increase the growth of cancers throughout the body, but despite years of investigation, they haven’t figured out exactly how this happens, or how to stop it.
SpaceX’s rumored “Starfall” program, related to its Starship initiative, aims to revolutionize in-space manufacturing, enabling advancements in various fields and reducing cargo transportation costs to unlock economic potential in space ## ## Questions to inspire discussion.
In-Orbit Manufacturing Potential.
🚀 Q: What unique advantages does in-orbit manufacturing offer? A: In-orbit manufacturing provides no gravity, perfect fluid flow, stable heat flow, and no air moving heat around, enabling growth of structures without scaffolding and benefiting industries like pharmaceuticals, advanced materials, and military logistics.
🏭 Q: Which industries could be disrupted by in-orbit manufacturing in the 2040s? A: In-orbit manufacturing could disrupt terrestrial industries in the 2040s, particularly pharmaceuticals, advanced materials, and military logistics, allowing production of high-value goods like protein crystals, retinal organoids, ZBLAN fiber, and semiconductor ingots in space.
Starfall Program.
🛰️ Q: What is SpaceX’s Starfall program? A: Starfall is a secret SpaceX program using small return pods from Starship to bring high-value goods back from orbit, potentially slashing the $40,000/kg cost of returning materials to Earth.
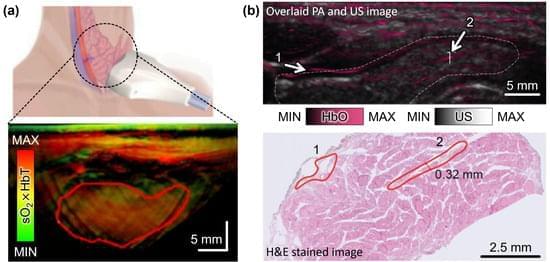
Photoacoustic imaging is a promising medical imaging modality that enables the visualization of molecular functional and morphological information of biological tissues. Its clinical potential has been widely investigated for assessing and diagnosing various diseases. Currently, several research groups are developing photoacoustic imaging systems for translation from the laboratory to the clinic. In particular, the integration of photoacoustic imaging into existing diagnostic ultrasound applications, such as cancer diagnosis, has shown promising results. Additionally, recent research has explored the application of photoacoustic imaging for novel clinical uses. In this review paper, recent trials of photoacoustic imaging in both conventional and novel clinical applications are summarized and evaluated.
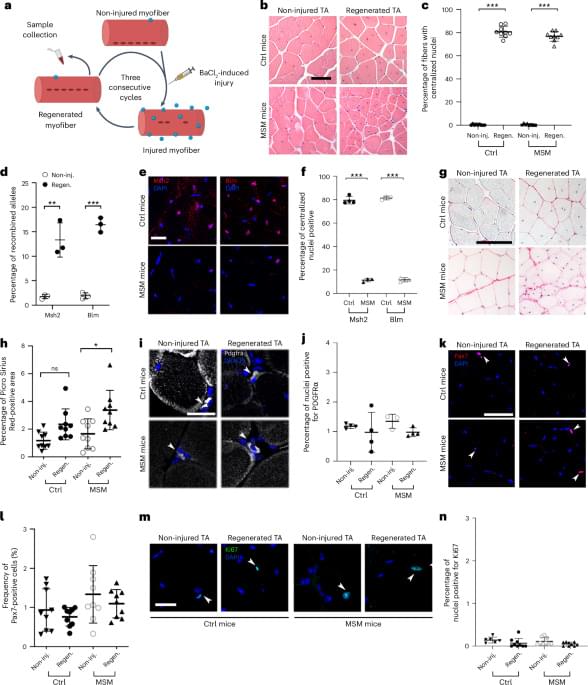
With aging, somatic mutations accumulate in cellular DNA; however, whether they drive age-related functional decline is incompletely understood. Here the authors show that these mutations can weaken muscle repair and reduce strength after injury, suggesting they play a role in age-related physical decline in mouse muscle.

Introduction Early detection of cardiovascular disease in primary care is a public health priority, for which the clinical and cost-effectiveness of an artificial intelligence-enabled stethoscope that detects left ventricular systolic dysfunction, atrial fibrillation and cardiac murmurs is unproven but potentially transformative.
Methods and analysis TRICORDER is a pragmatic, two-arm, multi-centre (decentralised), cluster-randomised controlled trial and implementation study. Up to 200 primary care practices in urban North West London and rural North Wales, UK, will be randomised to usual care or to have artificial intelligence-enabled stethoscopes available for use. Primary care clinicians will use the artificial intelligence-enabled stethoscopes at their own discretion, without patient-level inclusion or exclusion criteria.

The rare Antrodia cinnamomea fungus (also known as Taiwanofungus camphoratus) is only found in Taiwan, and is associated with one particular type of endangered tree. Long used for herbal medicines, the fungus has now been linked to cancer-fighting capabilities through a specific kind of sugar molecule.
Researchers from the National Taiwan University and National Yang Ming Chiao Tung University in Taiwan discovered the link by focusing on a group of compounds produced by the fungus called sulfate polysaccharides (SPS).
SPS is a kind of sugar molecule known as a sulfated galactoglucan, which combines compounds of glucose, galactose, and sulfate into one molecule.