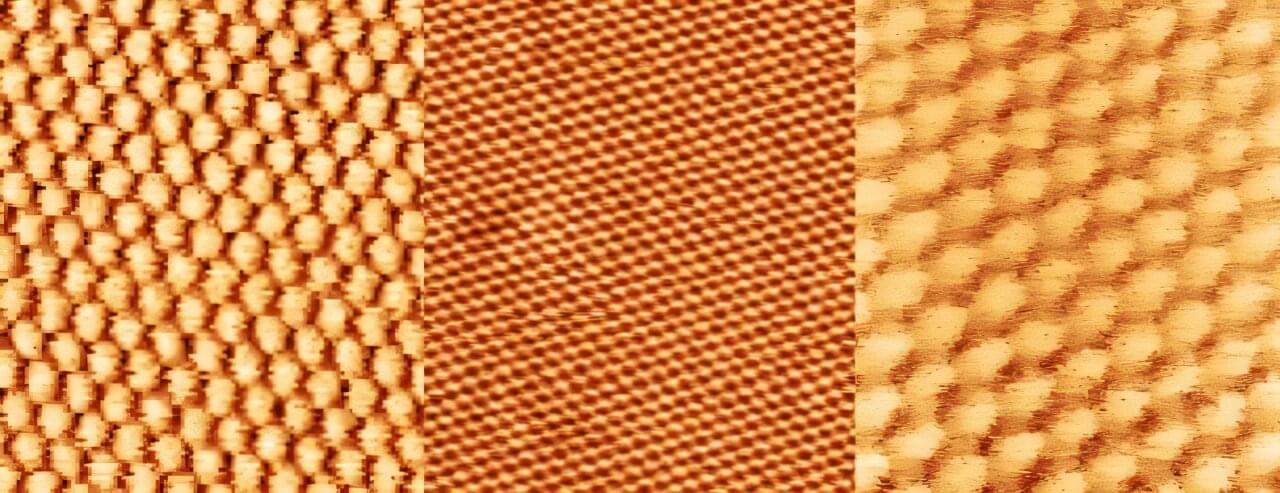
Nanomechanical systems developed at TU Wien have now reached a level of precision and miniaturization that will allow them to be used in ultra-high-resolution atomic force microscopes in the future. Their new findings are published in the journal Advanced Materials Technologies.
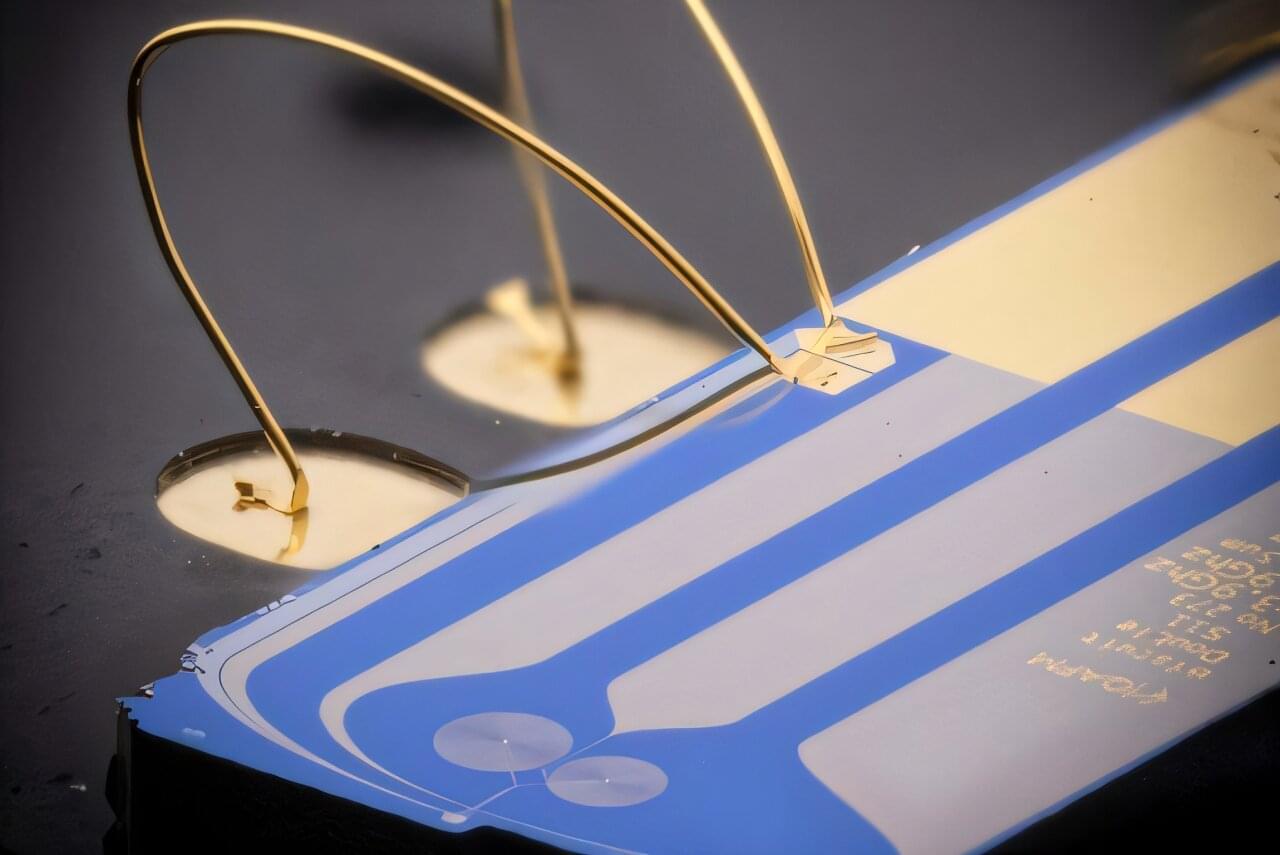
A major leap in measurement technology begins with a tiny gap of just 32 nanometers. This is the distance between a movable aluminum membrane and a fixed electrode, together forming an extremely compact parallel-plate capacitor—a new world record. This structure is intended for use in highly precise sensors, such as those required for atomic force microscopy.
But this world record is more than just an impressive feat of miniaturization—it is part of a broader strategy. TU Wien is developing various hardware platforms to make quantum sensing easier to use, more robust, and more versatile. In conventional optomechanical experiments, the motion of tiny mechanical structures is read out using light. However, optical setups are delicate, complex, and difficult to integrate into compact, portable systems. TU Wien therefore relies on other types of oscillations that are better suited for compact sensors.