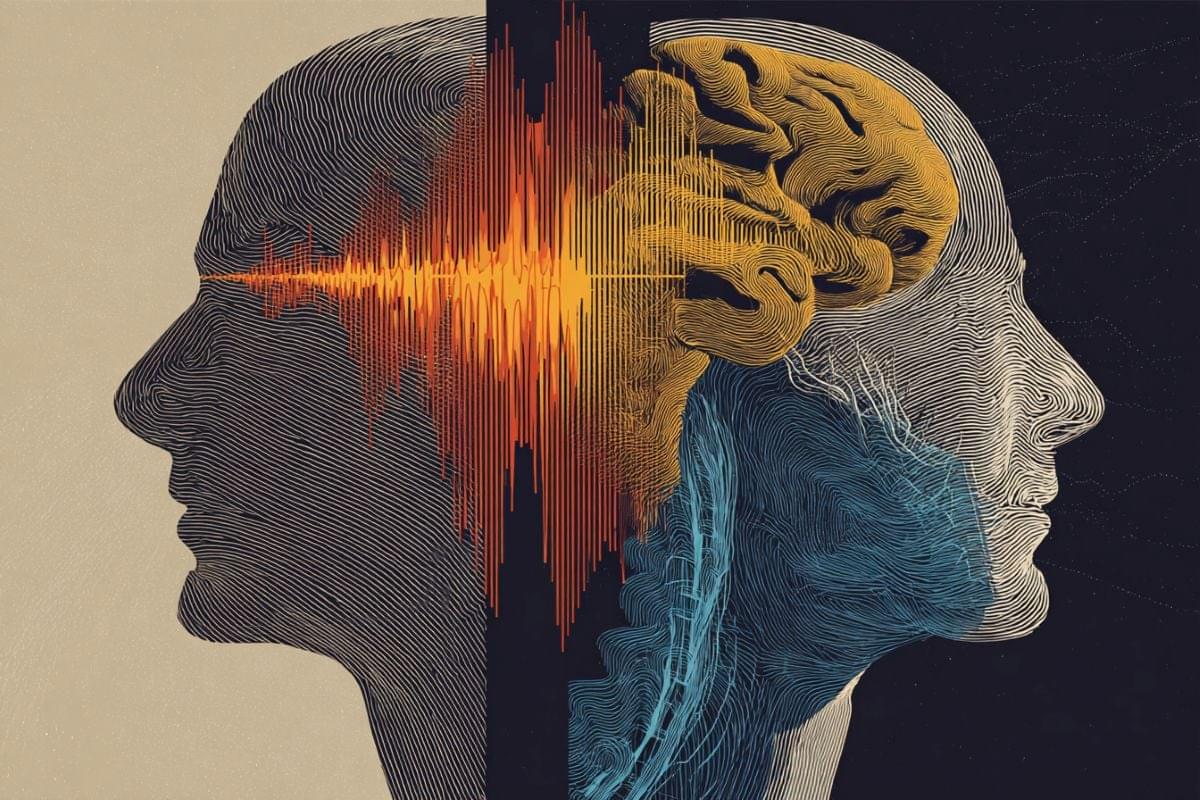
What does it mean that we have consciousness — and why does nature care that we do? In a remarkable new convergence of philosophy, psychology, and comparative neuroscience, researchers at Ruhr University Bochum argue that consciousness is not a mysterious luxury, but a powerful evolutionary adaptation.
According to their analysis, conscious experience first emerged as a mechanism of basic arousal — a primordial alarm system to protect living organisms from immediate danger. ([RUB Newsportal][1]) As evolution proceeded, consciousness evolved further: general alertness enabled organisms to filter through overwhelming flows of sensory data, focus selectively, and detect complex correlations — a capacity indispensable for learning, planning, and survival in a dynamic world.
Finally, in some lineages including our own, a third layer arose: reflexive, self-consciousness. This allows us not only to perceive the world, but to perceive ourselves — our bodies, thoughts, sensations — across time. With it comes memory, foresight, self-awareness, and the ability to integrate personal history into projects and social lives.
What is especially striking: these researchers show that consciousness need not depend on a “human-style” cortex. Studies of birds — whose brain architecture is very different from mammals — reveal comparable functional capacities: sensory awareness, integrated information processing, and even rudimentary forms of self-perception. ([RUB Newsportal][1]) This suggests that consciousness, far from being a human special-case, may be a widespread evolutionary solution — one that can arise in diverse biological substrates when the right functional constraints are met.
In this light, consciousness emerges not as an ineffable mystery or a metaphysical afterthought, but as a natural phenomenon with concrete functions: for feeling, for alertness, for learning, for self-representation. Understanding it may not only tell us who we are — but also why it ever made sense for life to become conscious.
Press Release: Ruhr University Bochum