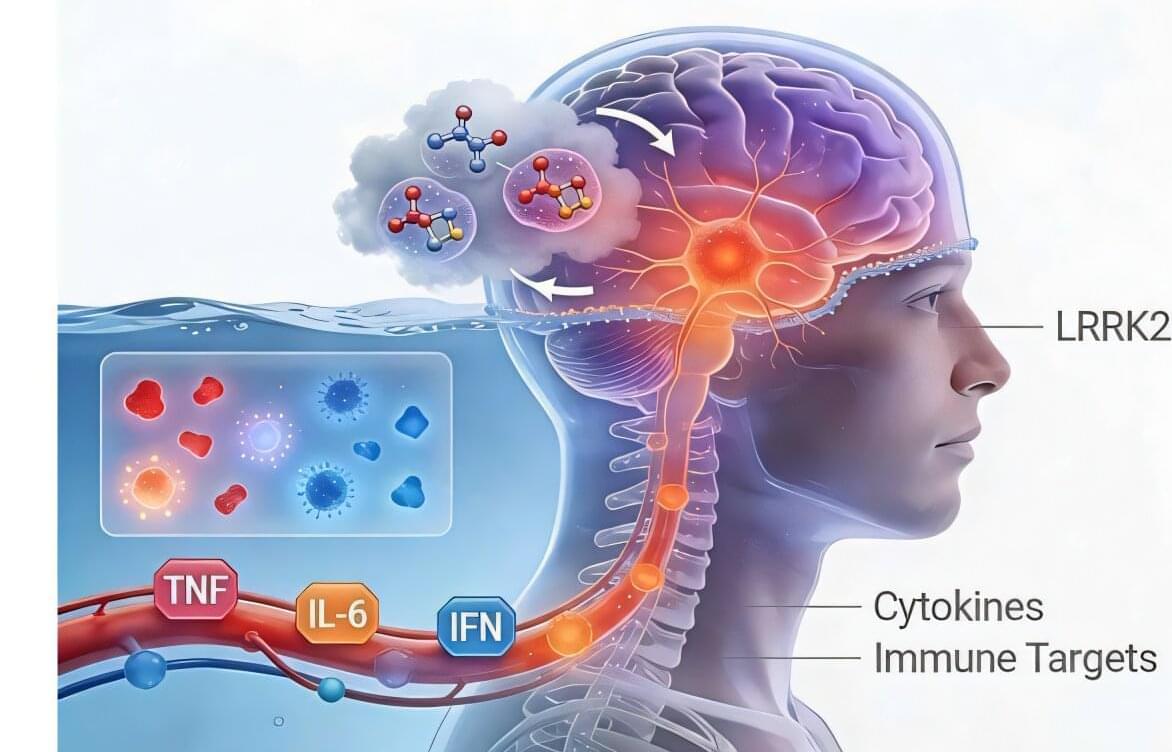
Enzymes are the molecular machines that power life; they build and break down molecules, copy DNA, digest food, and drive virtually every chemical reaction in our cells. For decades, scientists have designed drugs to slow down or block enzymes, stopping infections or the growth of cancer by jamming these tiny machines. But what if tackling some diseases requires the opposite approach?
Speeding enzymes up, it turns out, is much harder than stopping them. Tarun Kapoor is the Pels Family Professor in Rockefeller’s Selma and Lawrence Ruben Laboratory of Chemistry and Cell Biology. Recently, he has shifted the focus of this lab to tackle the tricky question of how to make enzymes work faster.
Already, his lab has developed a chemical compound to speed up an enzyme that works too slowly in people with a rare form of neurodegeneration. The same approach could open new treatment possibilities for many other diseases where other enzymes have lost function, including some cancers and neurodegenerative disorders such as Alzheimer’s.