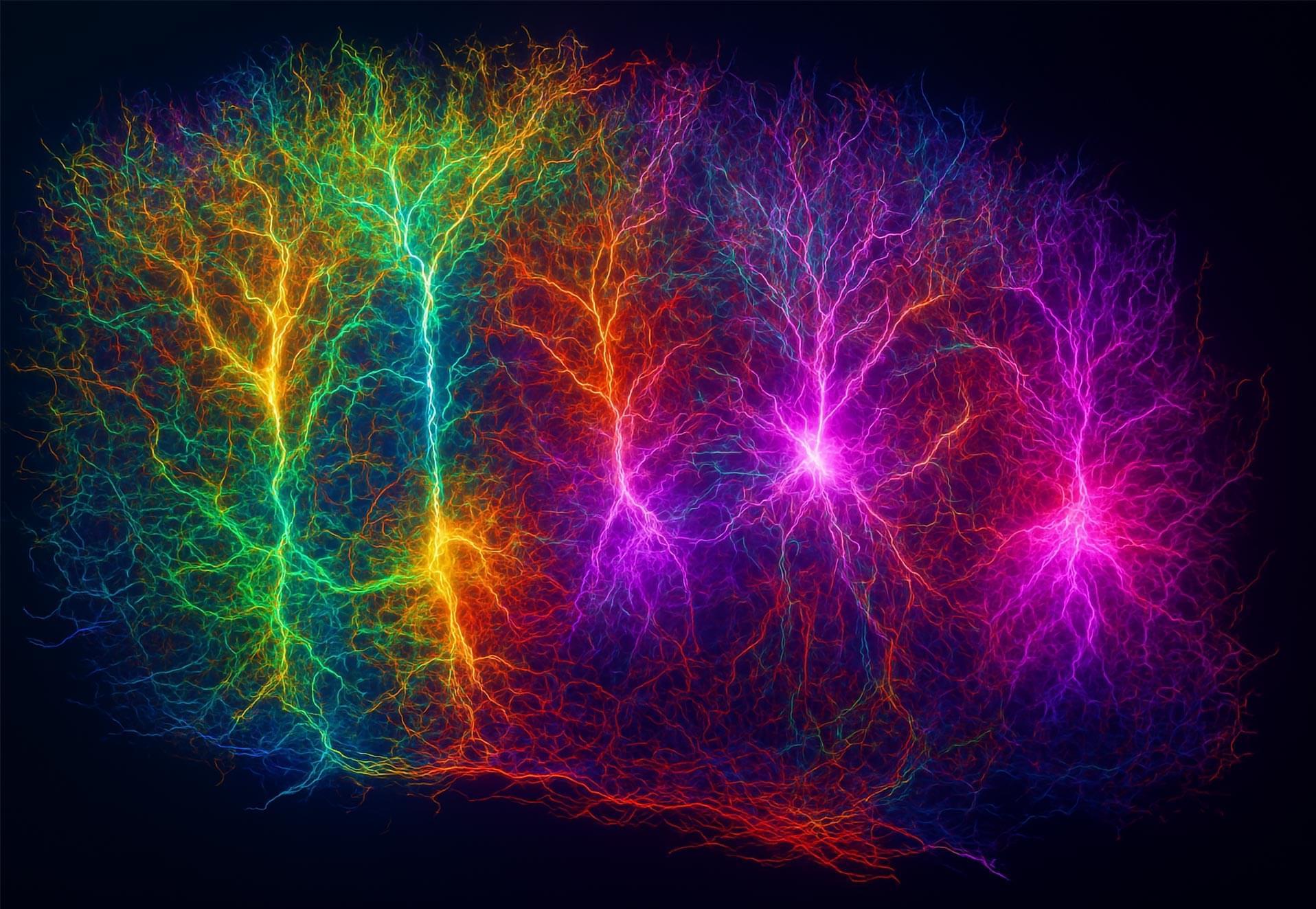
A team of engineers at Georgia Institute of Technology’s Wearable Intelligent Systems and Healthcare Center, working with colleagues affiliated with several institutions in South Korea, has developed a microscale brain–computer interface that is small enough to be placed between hair follicles on a user’s head.
In their paper published in the Proceedings of the National Academy of Sciences, the group describes how they made their interface, how it attaches to other hardware to allow readings to be captured and how well it worked during testing.
Over the past several decades, brain–computer interfaces have been developed that are capable of reading brain waves and responding to them in useful ways. These devices can be used to control a cursor on a computer screen, for example, or to choose buttons to press. Such devices are still in limited use, however, mainly due to their bulky nature. In this new effort, the researchers have developed a sensor so small it can be placed on the scalp between hair follicles.