You know that feeling when a song from your teenage years comes on, and suddenly you’re right back in your old bedroom, feeling everything as vividly as you did decades ago? Scientists call this the “reminiscence bump”—our strange tendency to form the most powerful, lasting emotional bonds with music we hear between ages 15 and 25. But until now, no one knew if this was just a Western phenomenon or if it looked the same for everyone, everywhere.
The study also revealed we’re not limited to just one “memory bump.” Three distinct patterns emerge: we connect with music our parents loved (cross-generational), music from our own coming-of-age years (the classic reminiscence bump), and music from recent years (the recency effect). Age and gender act like equalizers, turning up some bumps while fading others.
From the “reminiscence bump” to cross-generational musical connections, we’ll unpack the psychology and neuroscience behind your most meaningful playlists.
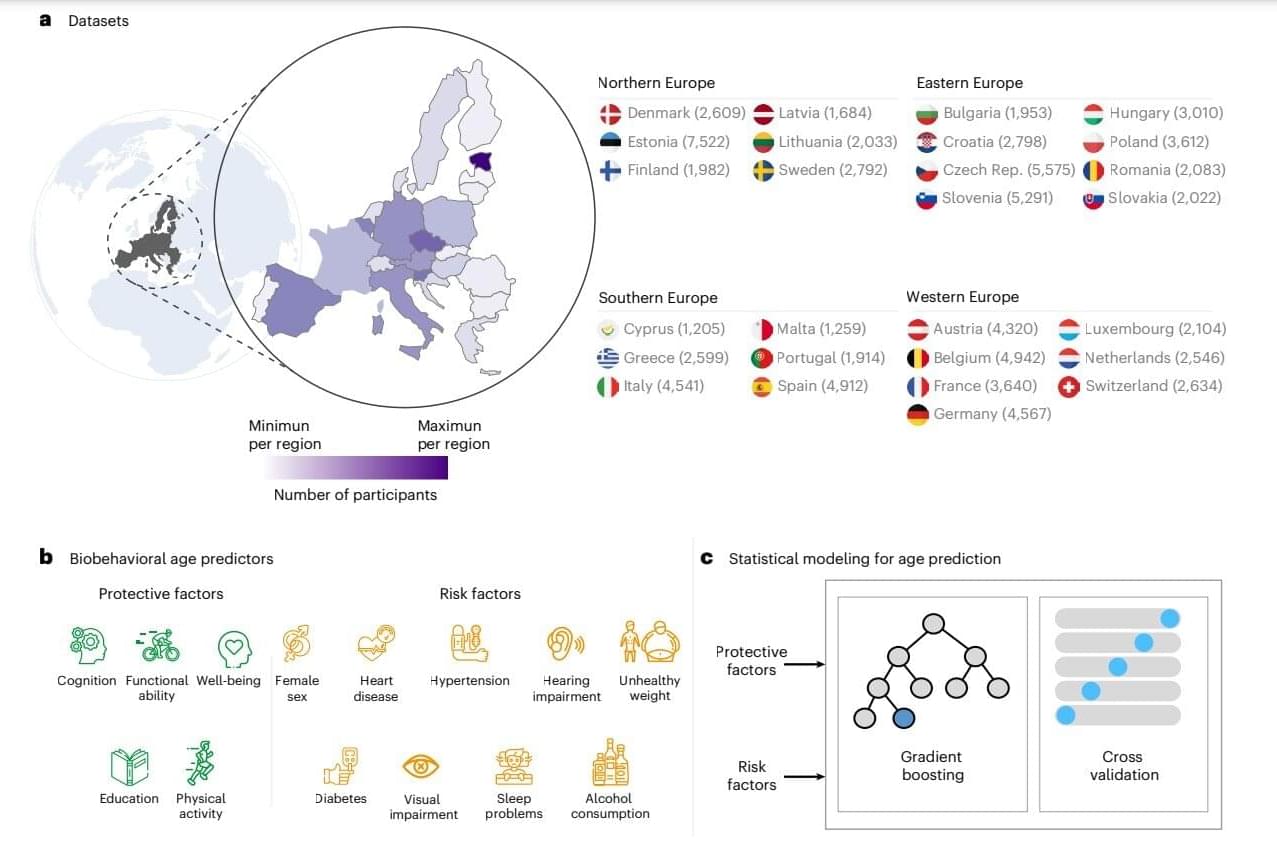
Some songs stay with us for a lifetime. Even decades later, a few familiar notes can unlock vivid memories. Yet the life periods from which these songs originate and their prominence across age and gender remain underexplored. This study examines lifespan patterns in music-related memory, focusing on age trends, gender differences, and the global presence of the “reminiscence bump”, a peak in emotional connection to music from adolescence and early adulthood. While this phenomenon is well-documented in Western samples, its global manifestation, gendered dimensions and variation across life stages remains unexplored. Using responses collected from 1891 participants across diverse geographical backgrounds, we analysed the release years of personally meaningful songs.