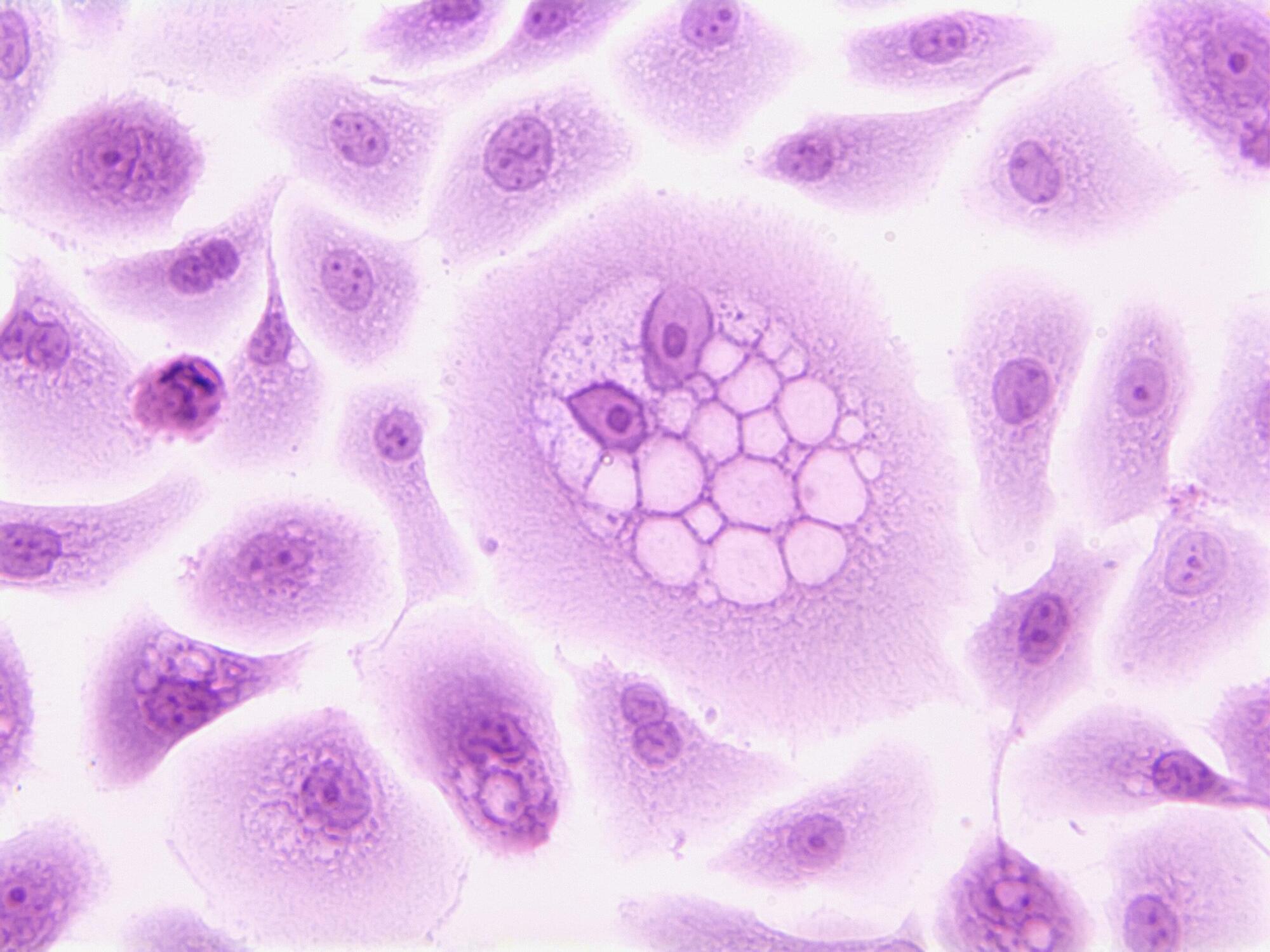
Cells have a remarkable housekeeping system: Proteins that are no longer needed, defective, or potentially harmful are labeled with a molecular “tag” and dismantled in the cellular recycling machinery. This process, known as the ubiquitin-proteasome system, is crucial for health and survival.
Now, an international team of scientists led by CeMM, AITHYRA and the Max Planck Institute of Molecular Physiology in Dortmund has identified a new class of small molecules that harness this natural system to accelerate the removal of an immune-modulating enzyme called IDO1.
The findings, published in Nature Chemistry, introduce a new concept in drug discovery that could transform how we target difficult proteins in cancer and beyond.