Scientists identify an important protein that increases “bacterial virulence,” when mutated, changing harmless bacteria to harmful ones.
As far as humans are concerned, bacteria can be classified as either harmful, pathogenic bacteria and harmless or beneficial non-pathogenic bacteria. To develop better treatments for diseases caused by pathogenic bacteria, we need to have a good grasp on the mechanisms that cause some bacteria to be virulent. Scientists have identified genes that cause virulence, or capability to cause disease, but they do not fully know how bacteria evolve to become pathogenic.
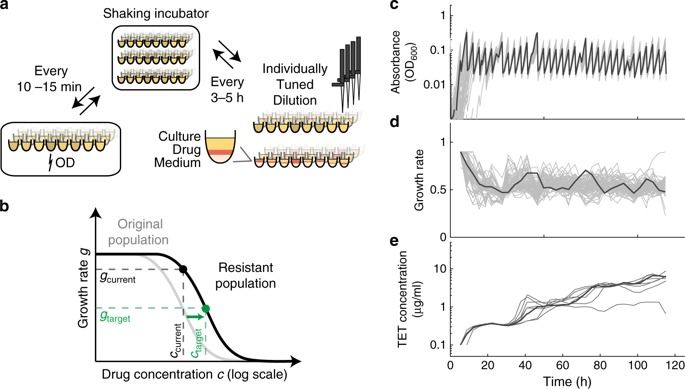
To find out, Professor Chikara Kaito and his team of scientists from Okayama University, Japan, used a process called experimental evolution to identify molecular mechanisms that cells develop to gain useful traits, and published their findings in PLoS Pathogens. “We’re excited by this research because no one has ever looked at virulence evolution of bacteria in an animal; studies before us looked at the evolution in cells,” said Prof Kaito.