Cancer is not a uniform disease. Rather, cancer is a disease of phenotypic plasticity, meaning tumor cells can change from one form or function to another. This includes reverting to less mature states and losing their normal function, which can result in treatment resistance, or changing their cell type altogether, which facilitates metastasis.
In addition to direct changes in your DNA in cancer, a key driver of cancer progression is where and when your DNA is activated. If your DNA contains the “words” that spell out individual genes, then epigenetics is the “grammar” of your genome, telling those genes whether they should be turned on or off in a given tissue. Even though all tissues in the body have almost exactly the same DNA sequence, they can all carry out different functions because of chemical and structural modifications that change which genes are activated and how. This “epigenome” can be influenced by environmental exposures such as diet, adding a dimension to how researchers understand drivers of health beyond the DNA code inherited from your parents.
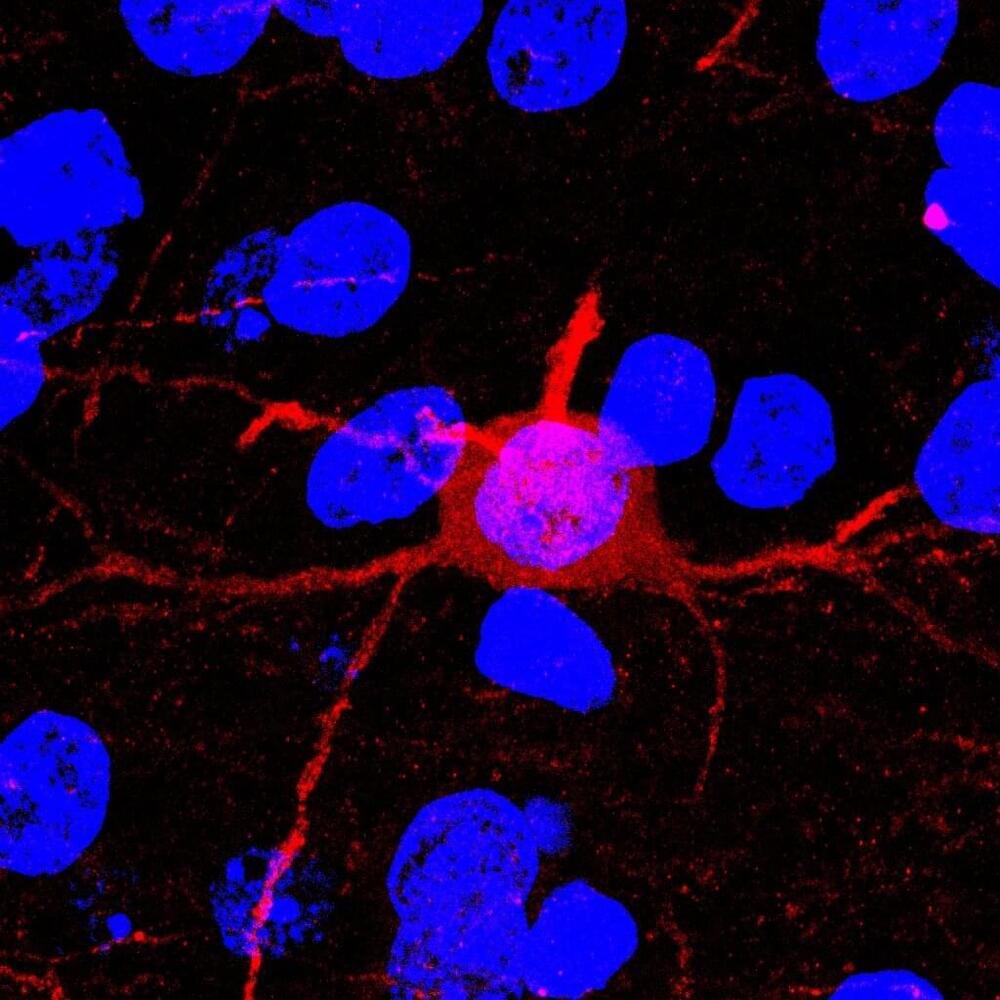
I’m a cancer researcher, and my laboratory at Johns Hopkins University studies how the differences among normal tissues are controlled by an epigenetic code, and how this code is disrupted in cancer. In our recently published review, colleague Andre Levchenko at Yale University and I describe a new approach to understanding cancer plasticity by combining epigenetics with mathematics. Specifically, we propose how the concept of stochasticity can shed light on why cancers metastasize and become resistant to treatments.