Year 2020 o.o!!!
The primary difficulty of interstellar communication is finding common ground between ourselves and other intelligent entities about which we can know nothing with absolute certainty. This common ground would be the basis for a universal language that could be understood by any intelligence, whether in the Milky Way, Andromeda, or beyond the cosmic horizon. To the best of our knowledge, the laws of physics are the same throughout the universe, which suggests that the facts of science may serve as a basis for mutual understanding between humans and an extraterrestrial intelligence.
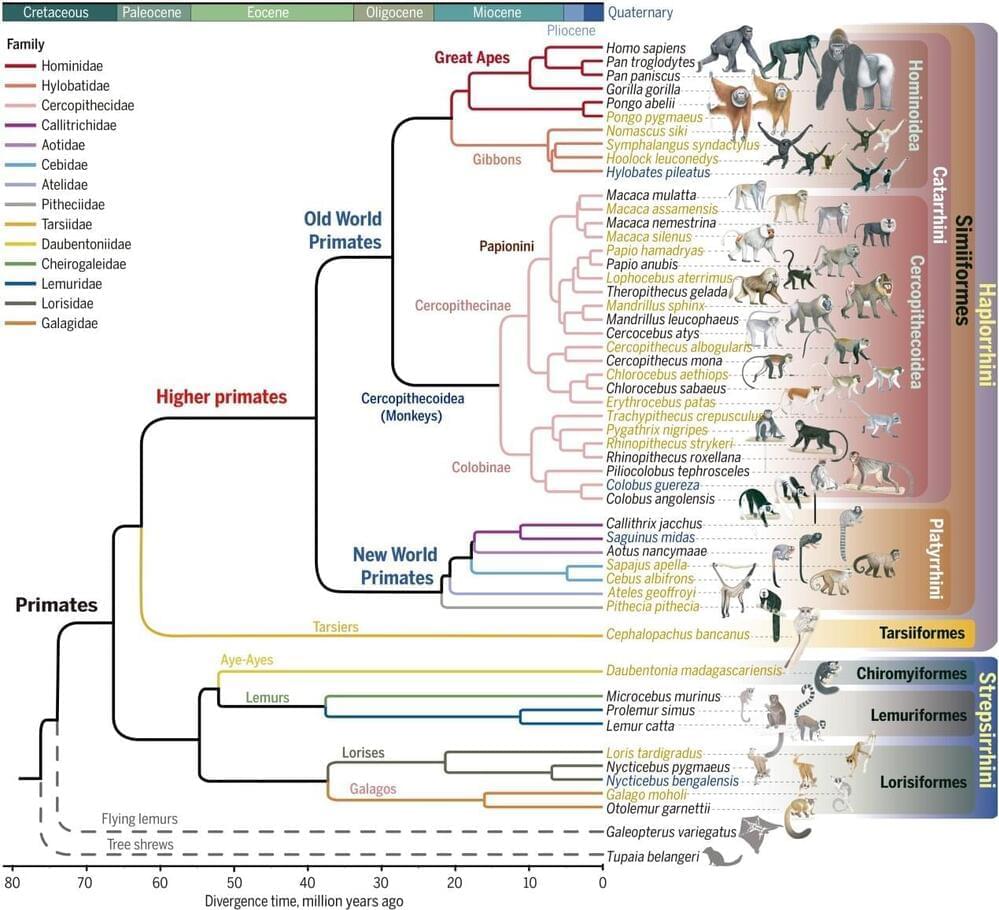
One key set of scientific facts presents an intriguing question. If aliens were to visit Earth and learn about its inhabitants, would they be surprised that such a wide variety of species all share a common genetic code? Or would this be all too familiar? There is probable cause to assume that the structure of genetic material is the same throughout the universe and that, while this is liable to give rise to life forms not found on Earth, the variety of species is fundamentally limited by the constraints built into the genetic mechanism.
On Earth we have only sequenced the genomes of a small percentage of living organisms and have only recently completed the human genome. We have successfully cloned several animals, but technical and ethical roadblocks prevent scientists from doing the same with humans. If an extraterrestrial civilization isn’t burdened with ethical dilemmas about cloning, however, sending the genetic code for humans and other species may be the most effective way to teach them about our biology.