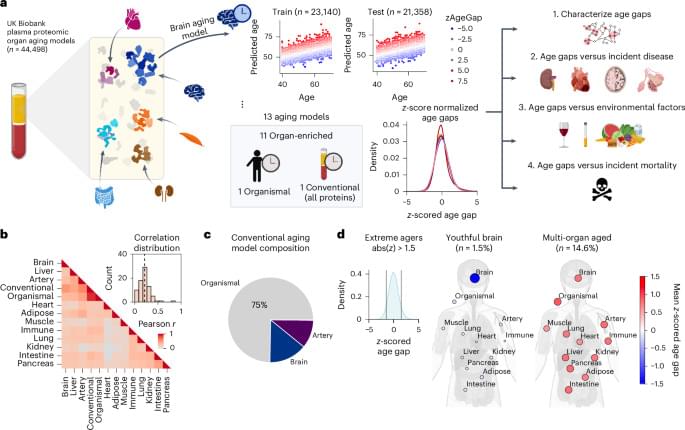
Potential treatments for amyotrophic lateral sclerosis (ALS) and other neurodegenerative diseases may already be out there in the form of drugs prescribed for other conditions. A team of researchers from Lawrence Livermore National Laboratory (LLNL), Stanford University and the University of California, Los Angeles (UCLA) are using artificial intelligence and machine learning (AI/ML) to try to find them.
Clinical trials for new drugs can take up to 5–7 years, so repurposing existing drugs is one of the best ways to deliver treatments quickly. AI/ML can make it even faster. By analyzing long-term electronic health records (EHRs) of patients with ALS, the team can identify drugs — or combinations of drugs — prescribed for other conditions that may influence the progression of the disease. The drugs’ “off-target” effects may not only affect patient survival but also provide insight into how neurodegenerative diseases work and inform better therapies.
“If you talk to any ALS caregiver, you will be moved because the disease has such a grim prognosis, so being able to do something is tremendously motivating,” said Priyadip Ray, a staff scientist in LLNL’s Computational Engineering Division (CED) who leads the effort.