A new drug prevents weight gain and fatty liver by controlling magnesium in cells. It made mice stay slim despite lifelong exposure to an unhealthy diet.




Researchers at the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) and Technical University of Vienna (TU Wien) have invented a new type of tunable semiconductor laser that combines the best attributes of today’s most advanced laser products, demonstrating smooth, reliable, wide-range wavelength tuning in a simple, chip-sized design.
Tunable lasers, or lasers whose light output wavelengths can be changed and controlled, are integral to many technologies, from high-speed telecommunications to medical diagnostics to safety inspections of gas pipelines.
Yet laser technology faces many trade-offs—for example, lasers that emit across a wide range of wavelengths, or colors, sacrifice the accuracy of each color. But lasers that can precisely tune to many colors get complicated and expensive because they commonly require moving parts.

“This is a huge step forward in the genetic treatment of deafness, one that can be life-changing for children and adults,” says Maoli Duan, consultant and docent at the Department of Clinical Science, Intervention and Technology, Karolinska Institutet, Sweden, and one of the study’s corresponding authors.
Gene therapy involved a synthetic adeno-associated virus (AAV) to deliver a functional version of the OTOF gene to the inner ear via a single injection through a membrane at the base of the cochlea called the round window. The injections were to target mutations in OTOF that can cause deficiencies of the otoferlin protein, that plays key roles in transmitting auditory signals.
According to the researchers, the effects of the gene therapy were rapid, and the majority of the participants recovered some hearing after one month. At a 6-month follow-up, all participants showed considerable improvements, with the average perceptible volume of sound improving from 106 decibels to 52 decibels.

A large urogenital hiatus in level III results in a higher risk of developing pelvic organ prolapse after birth and failure after prolapse surgery. Deepening of the pelvic floor and downward rotation of the levator plate have also been linked to prolapse. Currently we lack data that evaluates how these measures relate to one another and to prolapse occurrence and size.
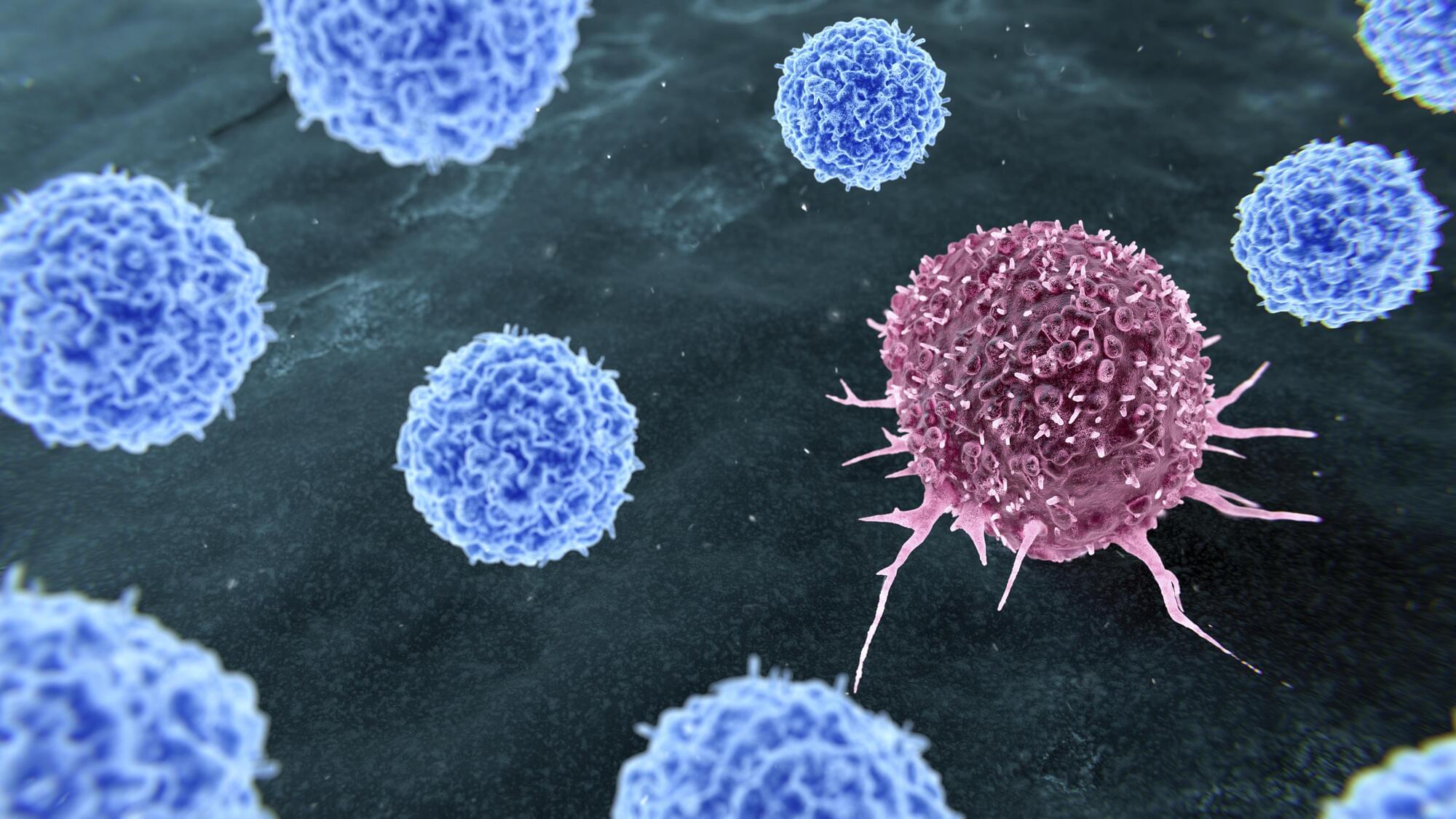
Researchers in Sheffield Hallam University’s Biomolecular Sciences Research Centre, in partnership with Paxman, have discovered that combining scalp cooling treatment with antioxidants can significantly reduce or even prevent the damage to hair follicles caused by chemotherapy drugs. This breakthrough has the potential to enhance and standardise scalp cooling efficacy levels, potentially transforming it into a more consistent and universally reliable method.
Led by Dr Nik Georgopoulos, the study uses human keratinocytes and hair follicle cultures to test the effects of cooling and antioxidants on chemotherapy-treated cells. The research was the culmination of years of work in partnership with the Paxman Scalp Cooling Research Centre.
The paper, which has been published today (Tuesday 8 July) in the journal Frontiers of Pharmacology, showed for the first time that.
New breakthrough in preventing chemotherapy-induced hair loss and could make a real difference to the lives of cancer patients worldwide.

A blood-test analysis developed at Stanford Medicine can determine the “biological ages” of 11 separate organ systems in individuals’ bodies and predict the health consequences.
Researchers in Chicago believe they’ve found a virus that could be a trigger for Parkinson’s disease.
Parkinson’s impacts millions of people in the United States, according to Northwestern Medicine, and while some cases are linked to genetics, most cases are not.

When people take antibiotics, some of the dose is excreted with urine and feces and ends up in our wastewater. The presence of this low dose of antibiotic creates an opportunity for resistant bacteria to evolve.
Scientists studying antibiotic-resistant bacteria in wastewater at a treatment plant discovered multi-drug-resistant strains of bacterial species which are usually not dangerous to healthy people, but which could transmit genes for antibiotic resistance to much more dangerous bacteria like E. coli.
The scientists then challenged the bacteria with natural compounds which could potentially be included in wastewater treatment to kill off bacteria and fight antibiotic resistance. The most effective were curcumin, which comes from turmeric, and emodin, from rhubarb.