Combining self-assembly techniques from across scientific disciplines could allow us to precisely build any material structure.
Nanocars are an impressive achievement – but nanoarchitectonics can unlock a far greater range of material structures.
In a lecture at the American Physical Society in 1959 titled ‘There’s Plenty of Room at the Bottom’, Richard Feynman argued that huge possibilities come from working in the world of molecules and atoms. He dreamed of ultra-small computers, cars running under a microscope, and medical machines working in our body.
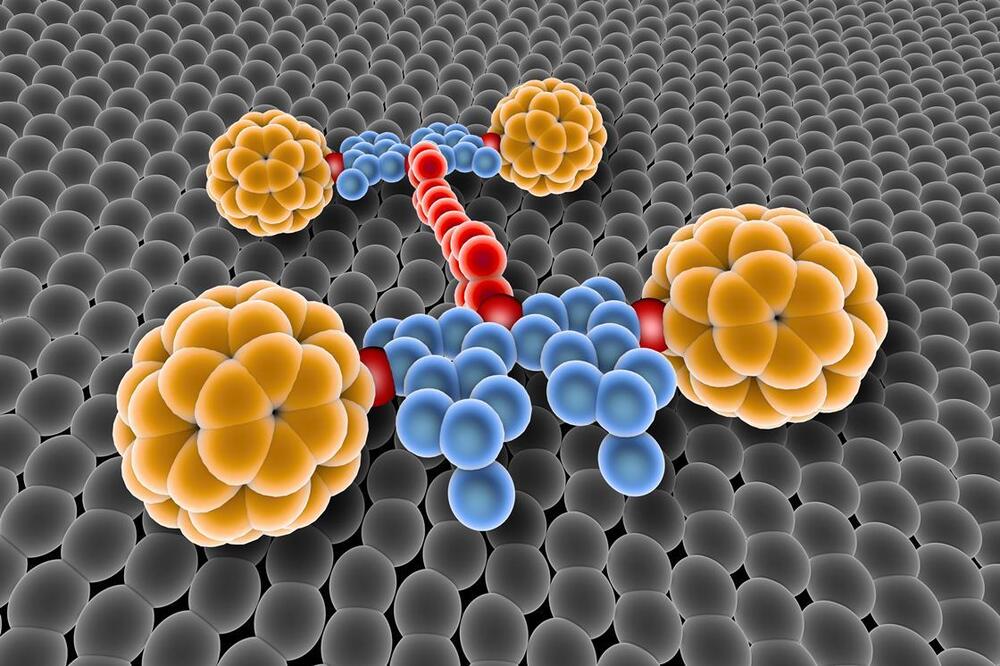
These dreams are now coming true. In 2017, we had the first World Nanocar Race in Toulouse, France. Six teams from around the world manipulated nanometre-size cars to run on a metal surface under a scanning tunnelling microscope. A nanocar is 2 billion times smaller than a usual car, corresponding to the size difference between a rice grain and the Earth. Feynman only imagined cars 4000 times smaller than normal. However, few of the nanocars resembled cars, and none were powered by their own motors. There’s still plenty of room for improvement.