Before too long, you may be able to buy a breath mint that rebuilds your tooth enamel while it whitens your teeth, thanks to a team of University of Washington researchers.
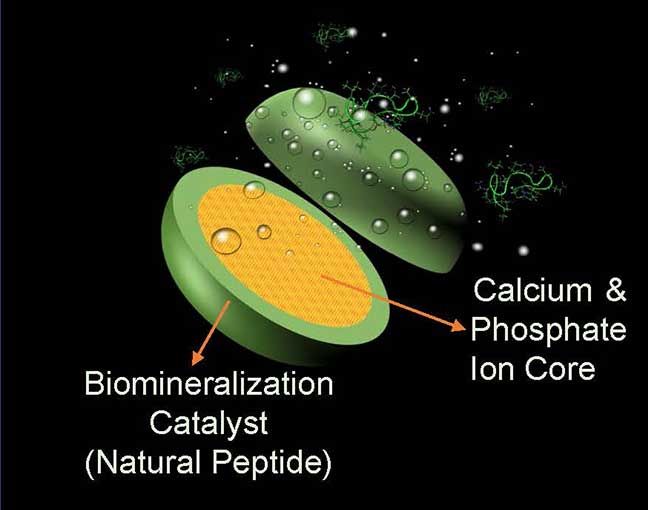
The team is preparing to launch clinical trials of a lozenge that contains a genetically engineered peptide, or chain of amino acids, along with phosphorus and calcium ions, which are building blocks of tooth enamel. The peptide is derived from amelogenin, the key protein in the formation of tooth enamel, the tooth’s crown. It is also key to the formation of cementum, which makes up the surface of the tooth root.
Each lozenge deposits several micrometers of new enamel on the teeth via the peptide, which is engineered to bind to the damaged enamel to repair it while not affecting the mouth’s soft tissue. The new layer also integrates with dentin, the living tissue underneath the tooth’s surface. Two lozenges a day can rebuild enamel, while one a day can maintain a healthy layer. The lozenge – which can be used like a mint – is expected to be safe for use by adults and children alike.