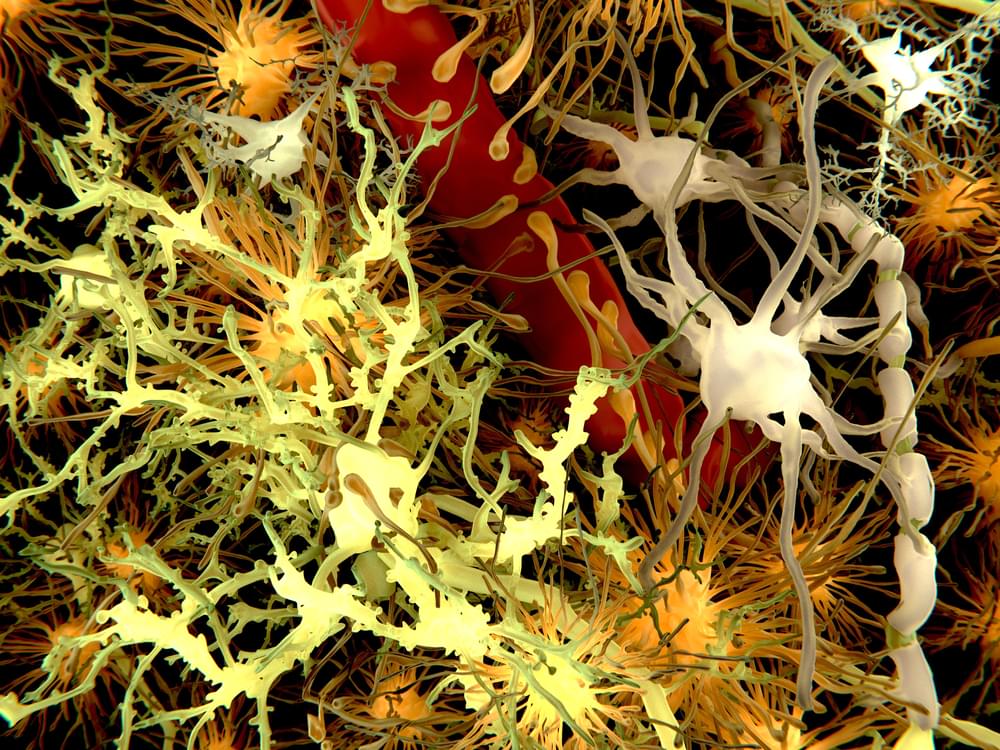
He suffered both physical and mental long-term side effects.
In April of 2006, doctors from London University revealed a case study of what they believed at the time was the largest amount of ecstasy ever consumed by a single person. They published a case report of a British man named only Mr. A estimated to have taken around 40,000 pills of MDMA over nine years, the most amount known to anyone.
They reported that the man then suffered from prominent physical and mental health side effects, such as extreme memory problems, paranoia, hallucinations and depression, as well as painful muscle rigidity around his neck and jaw, which often prevented him from opening his mouth.
Fpm/iStock.
Now, a new interview with the British style magazine The Face has surfaced where Dr. Christos Kouimtsidis, a psychiatrist who coauthored the case study, explains why the man’s story is still so fascinating after all these years.