This is true. I’ve been missing photography and books. Too much YouTube even can give you a bit of depression and anxiety. I’m a YouTube addict I’ll admit.
Reducing social media usage by as little as 15 minutes per day can increase health and well-being, claims a new study published in the Journal of Technology in Behavioral Science. The findings indicate that a 15-minute reduction in social media usage has positive consequences for one’s social life, vitality, and health.
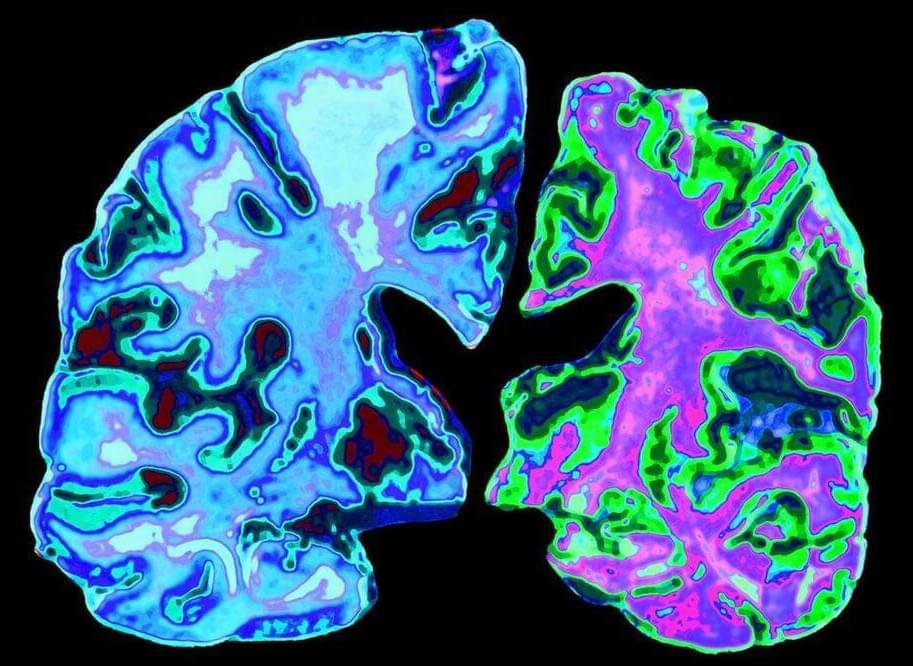
Research has shown that excessive social media use can lead to a range of negative outcomes, including increased feelings of loneliness, anxiety, and depression. Social media use has also been linked to poor sleep quality, decreased physical activity, and decreased face-to-face social interaction. These negative outcomes are particularly concerning given that young adults are among the heaviest social media users, with many spending several hours daily on social media platforms.
Despite the growing concern about the negative effects of social media use, there is limited research on the effectiveness of interventions aimed at reducing social media use. Previous studies have suggested reducing social media use can improve mental health outcomes. However, small sample sizes and reliance on self-reported measures of social media use and mental health outcomes have limited these studies.