Huntington’s disease is a genetic disorder that is caused by an unusual number of repeats in the huntingtin gene; there make the gene too long, and lead to the production of a toxic protein in brain cells. Symptoms of the disease tend to arise when a person is in their 30s or 40s and it is typically fatal within 20 years. New work may change that, however.
Category: neuroscience – Page 57

Scientists Identify Brain Signal Disruptions Behind Voices in Schizophrenia
A new study reveals a missing area of brain activity in the minds of people with schizophrenia who hear voices.
The analysis of brain wave data suggests a combination of two neurological functions could trigger auditory verbal hallucinations.
Researchers from China found evidence of a breakdown in the ability to prepare the senses for specific words to be spoken. This on its own, however, isn’t enough; another area that filters our brain’s internal chatter is also enhanced in those with schizophrenia who experience unsettling auditory hallucinations.
In a first, scientists observe short-range order in semiconductors
Inside the microchips powering your devices, atoms aren’t just randomly scattered. They follow a hidden order that can change how semiconductors behave.
A team of researchers from the Lawrence Berkeley National Laboratory (Berkeley Lab) and George Washington University has, for the first time, observed these tiny patterns, called short-range order (SRO), directly in semiconductors.
This discovery is a game-changer, as understanding how atoms naturally arrange themselves could let researchers design materials with desirable electronic properties. Such control could revolutionize quantum computing, neuromorphic devices that mimic the brain, and advanced optical detectors.
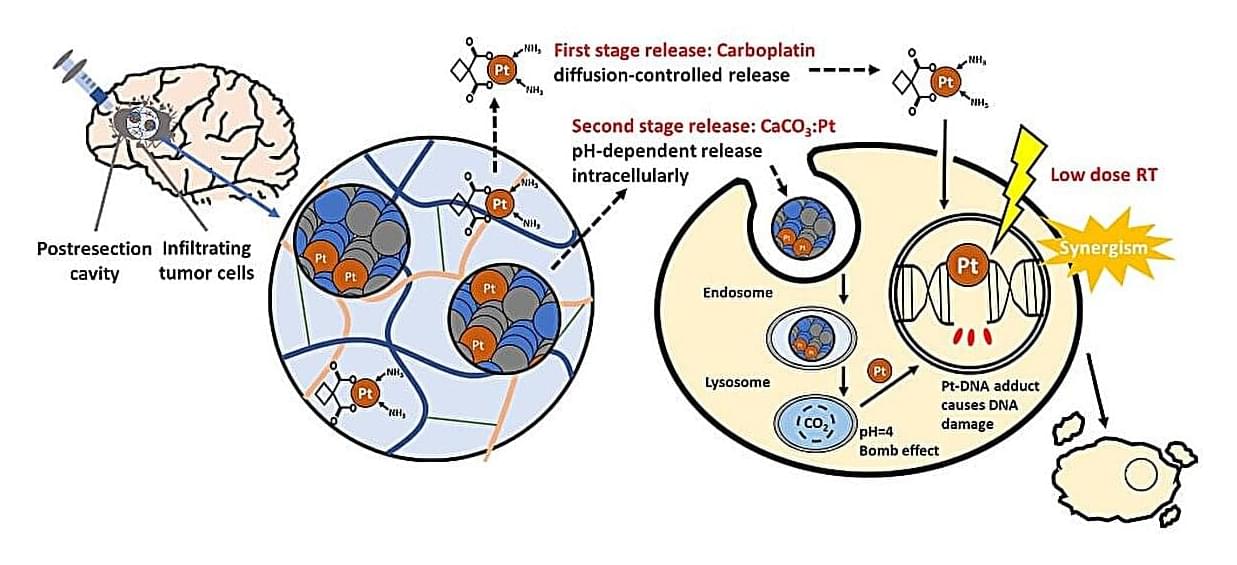
Time-released gel packs a one-two punch against aggressive brain tumors
High-grade gliomas are aggressive brain tumors with poor prognosis, largely because even after surgical removal, infiltrative residual tumor cells often regrow during the latency before radiotherapy, leading to recurrence. The standard chemoradiotherapy only modestly improves survival. A crucial window of vulnerability arises post-surgery, before radiotherapy begins, where residual tumor cells are not well addressed by systemic chemotherapy.
Prof. Feng-Huei Lin and Dr. Jason Lin from National Taiwan University have designed a local post-surgical gel packing with sequential delivery of platinum agents that could maintain therapeutic drug concentrations intracranially and synergize with subsequent radiotherapy to eliminate glioma tissue. Their study is published in the Chemical Engineering Journal.
The cutting-edge drug-delivery gel can be directly injected into the surgical cavity following tumor resection. This gel provides sustained local delivery of platinum-based anticancer agents, ensuring effective eradication for residual glioma tissue that remain after surgery. The gel is designed to maximize the therapeutic impact while minimizing systemic exposure.

How the brain decides which moments you’ll never forget
Boston University researchers found that ordinary moments can gain staying power if they’re connected to significant emotional events. Using studies with hundreds of participants, they showed that the brain prioritizes fragile memories when they overlap with meaningful experiences. This could help explain why we recall certain details surrounding big events and may lead to new ways of boosting learning and treating memory disorders.
New Study Finds Evidence of Hepatitis C Virus in Cells Lining Human Brain
Observational studies of psychiatric diseases such as schizophrenia, bipolar disorder and major depression have long tied viral infections with behavioral symptoms in these disorders, but scientists have been unable to find direct evidence of suspected viruses in the brain. Experts say that’s possibly because viruses may not get directly inside the brain, but may target the brain lining instead.
After testing that idea using postmortem human brain samples and the electronic medical records of 285 million patients, a team of Johns Hopkins Medicine scientists says it has found such evidence in the form of the liver-damaging hepatitis C virus in the human brain’s choroid plexus, a collection of cells that make up the lining of the fluid-filled cavities, or ventricles, and — notably — produce the cerebrospinal fluid that protects the brain and spinal cord…
…’Our findings show that it’s possible that some people may be having psychiatric symptoms because they have an infection, and since the hepatitis C infection is treatable, it might be possible for this patient subset to be treated with antiviral drugs and not have to deal with psychiatric symptoms,’ Sabunciyan says.
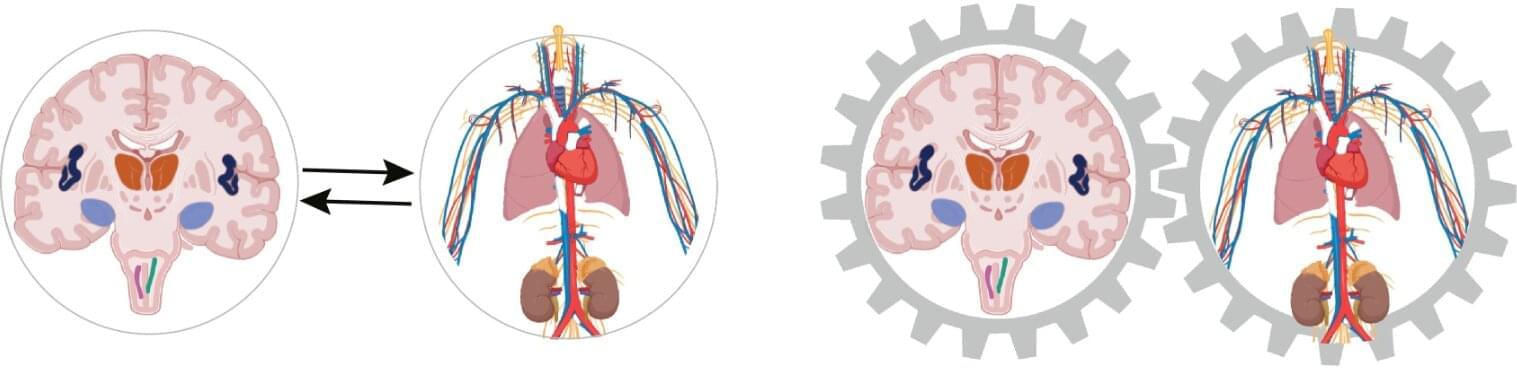
Growing evidence that the heart has a strong influence on thinking and feeling
The influence of the heart and circulatory system occurs within milliseconds, and every single heartbeat plays a role. The role of the heart in the psyche and cognition is evident in the high coincidence of cardiovascular diseases, such as high blood pressure and heart attack, and mental illnesses, such as depression and anxiety disorders.
There are a number of explanations for this high coincidence, but none of them have been definitively proven yet. For example, negative psychological reactions to a diagnosis of cardiovascular disease are cited as a reason for the development of mental illness. On the other hand, an unhealthy lifestyle in the presence of mental illness is considered a risk factor for the development of cardiovascular disease.
The concept is based on integrated brain–body states. Every physical process, such as a heartbeat or any change in blood pressure or metabolism, is automatically accompanied by a mental or psychological process. This means that the two are inextricably linked.

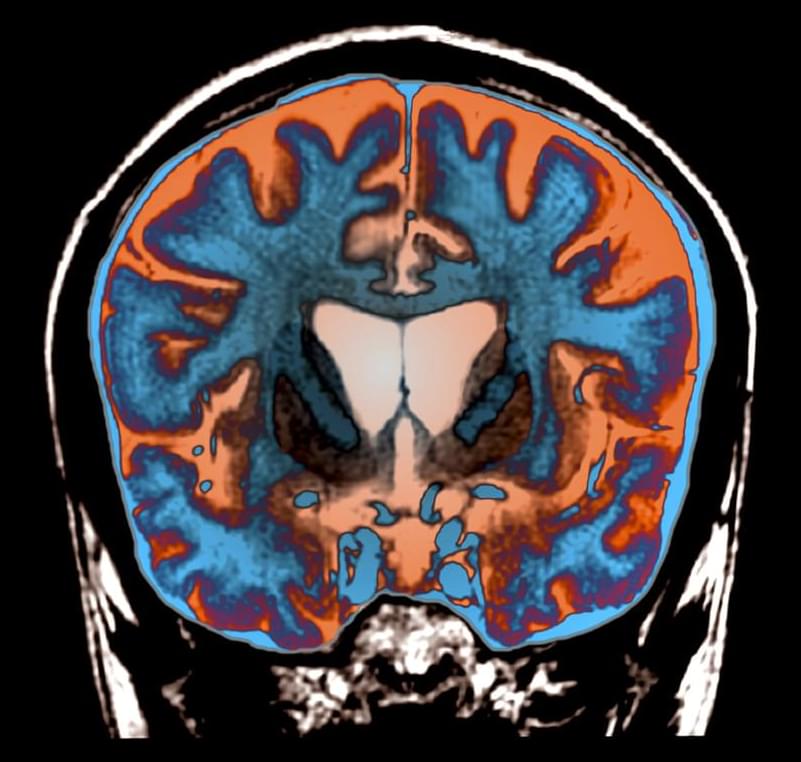
Chronic Insomnia May Spark Changes in The Brain That Trigger Dementia
Staring at the ceiling while the clock blinks 3am doesn’t only sap energy for the next day. A large, long-running US study of older adults has now linked chronic insomnia to changes inside the brain that set the stage for dementia.
The researchers, from the Mayo Clinic in the US, followed 2,750 people aged 50 and over for an average of five and a half years. Every year the volunteers completed detailed memory tests and many also had brain scans that measured two telltale markers of future cognitive trouble: the buildup of amyloid plaques, and tiny spots of damage in the brain’s white matter – known as white-matter hyperintensities.
Participants were classed as having chronic insomnia if their medical records contained at least two insomnia diagnoses a month apart – a definition that captured 16 percent of the sample.
Free Will, Quantum & Orchestrated Objective Reduction
An extended exploration of what science tells us about free will and consciousness in a quantum universe, including Sir Roger Penrose’s theory of Orchestrated Objective Reduction.
Watch my exclusive video ISRU: https://nebula.tv/videos/isaacarthur–…
Get Nebula using my link for 40% off an annual subscription: https://go.nebula.tv/isaacarthur.
Get a Lifetime Membership to Nebula for only $300: https://go.nebula.tv/lifetime?ref=isa…
Use the link gift.nebula.tv/isaacarthur to give a year of Nebula to a friend for just $30.
Join this channel to get access to perks:
/ @isaacarthursfia.
Visit our Website: http://www.isaacarthur.net.
Support us on Patreon: / isaacarthur.
Support us on Subscribestar: https://www.subscribestar.com/isaac-a…
Facebook Group: / 1583992725237264
Reddit: / isaacarthur.
Twitter: / isaac_a_arthur on Twitter and RT our future content.
SFIA Discord Server: / discord.
Episode 353a, June 30, 2024 Written, Produced & Narrated by Isaac Arthur.
Music Courtesy of Epidemic Sound http://epidemicsound.com/creator.
Select imagery/video supplied by Getty Images.
Huntington’s progression slowed by experimental gene therapy
Even hearing the phrase “Huntington’s disease” will make a room suddenly somber. So the joy that accompanied a recent announcement of results of an experimental gene therapy for the deadly diseases signaled an unfamiliar sense of hope.
In a small clinical trial, brain injections of a virus that codes for a tiny segment of RNA may have prevented the formation of the rogue proteins that make Huntington’s so devastating. The early results, announced September 24 in a news release, show that over three years, the treatment slowed Huntington’s progression by up to 75 percent. While not a cure, the treatment could potentially give people living with Huntington’s disease, who might otherwise face early disability and death, the gift of many more years of life.