A new study hints that age-related changes in our brains may explain why time feels like it’s slipping away faster with every passing year.

A large international study involving nearly 700 participants reveals that women with a precursor condition to Parkinson’s disease show significantly less brain atrophy—decreased cortical thickness in the brain—than men, despite similar clinical severity. This discovery, published in the journal Nature Communications, could lead scientists to explore the role that hormones might play in treating the disease.
Isolated REM sleep behavior disorder is characterized by violent movements during sleep, where people literally “act out” their dreams. Far from being harmless, this disorder is the most reliable early warning sign of neurodegenerative diseases caused by the accumulation of a toxic protein in the brain: more than 70% of affected individuals will eventually develop Parkinson’s disease, Lewy body dementia, or, more rarely, multiple system atrophy (a disease affecting multiple body systems).
“This sleep disorder offers a unique window of opportunity to study the mechanisms of neurodegeneration before major motor or cognitive symptoms appear,” explains Shady Rahayel, professor at UdeM’s Faculty of Medicine and leader of this study.
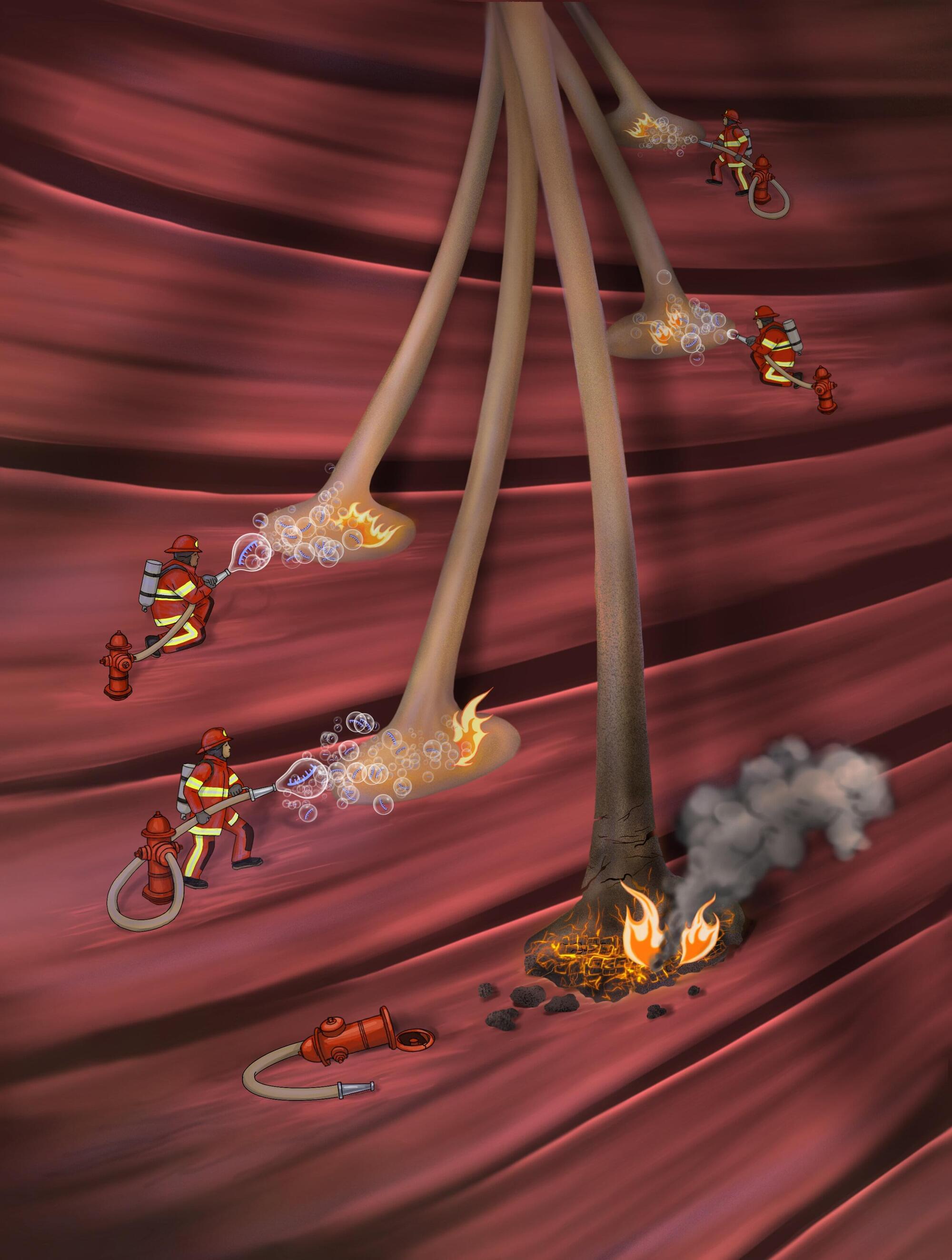
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease characterized by progressive muscle wasting and limb paralysis. This neurodegenerative condition results from the gradual destruction of motor neurons, the nerve cells that control muscles.
Past neuroscience studies have identified a TAR DNA-binding protein that plays a key role in ALS, known as TDP-43. This protein, which generally regulates RNA processing (i.e., how genetic information is managed inside cells), was found to abnormally accumulate in the axons (i.e., nerve fibers) of patients diagnosed with ALS.
Researchers at Tel Aviv University, Sheba Medical Center and other institutes carried out a study aimed at further exploring the mechanisms that underpin this local aggregation of TDP-43 in axons.
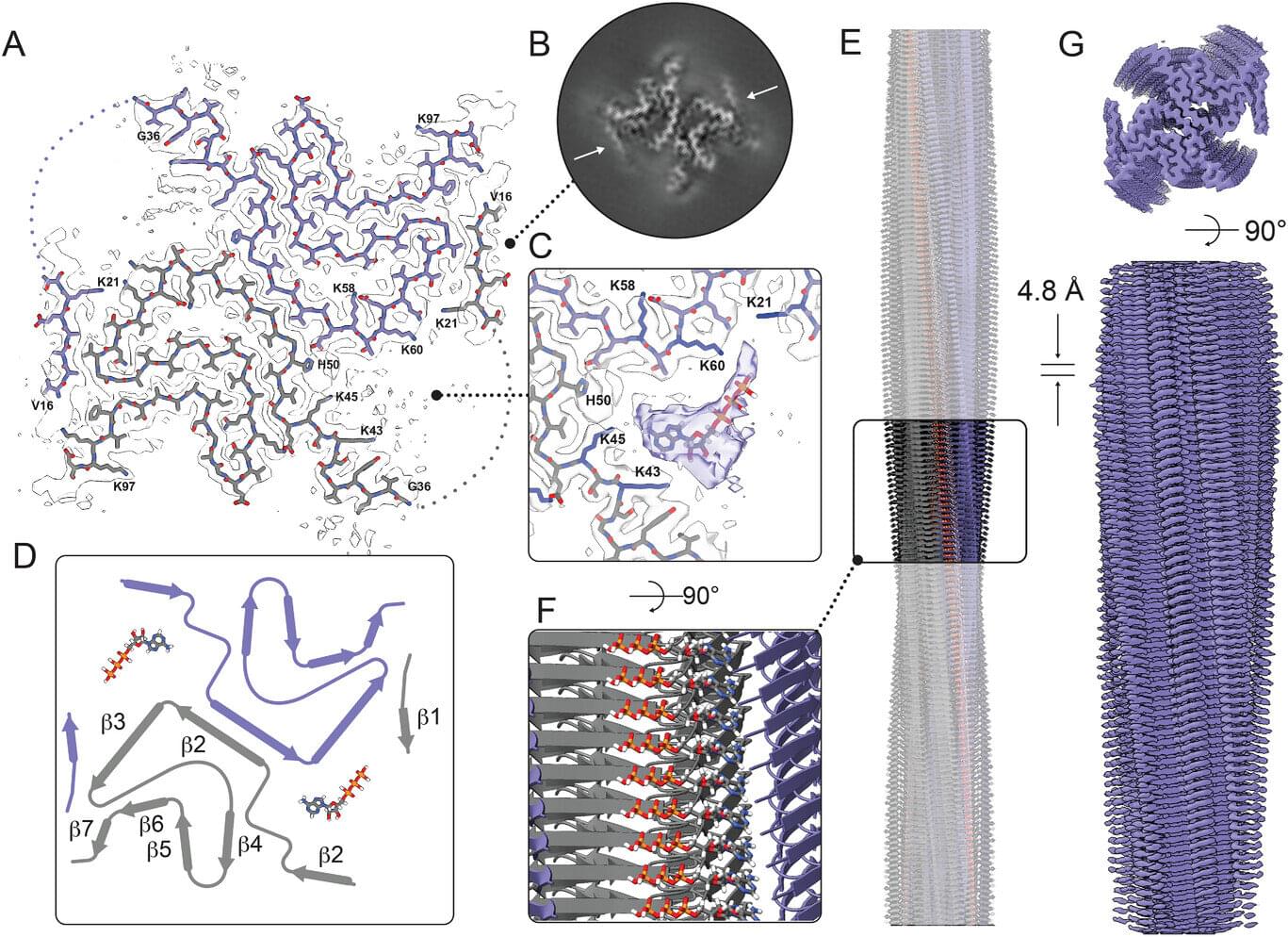
A new study led by Rice University’s Pernilla Wittung-Stafshede has revealed that protein clumps, or plaques that clog the brain, associated with Parkinson’s disease are not merely waste; they can actively drain energy from brain cells. These clumps, composed of a protein called alpha-synuclein, were found to break down adenosine triphosphate (ATP), the molecule responsible for powering nearly all cellular activities.
Published in Advanced Science, the research demonstrates that when ATP binds to these clumps, the protein reshapes itself to trap the molecule in a small pocket. This process causes ATP to break apart and release energy, functioning similarly to an enzyme.
This unexpected finding could change scientists’ understanding of the damage caused by these clumps, which are hallmarks of diseases such as Parkinson’s and Alzheimer’s.
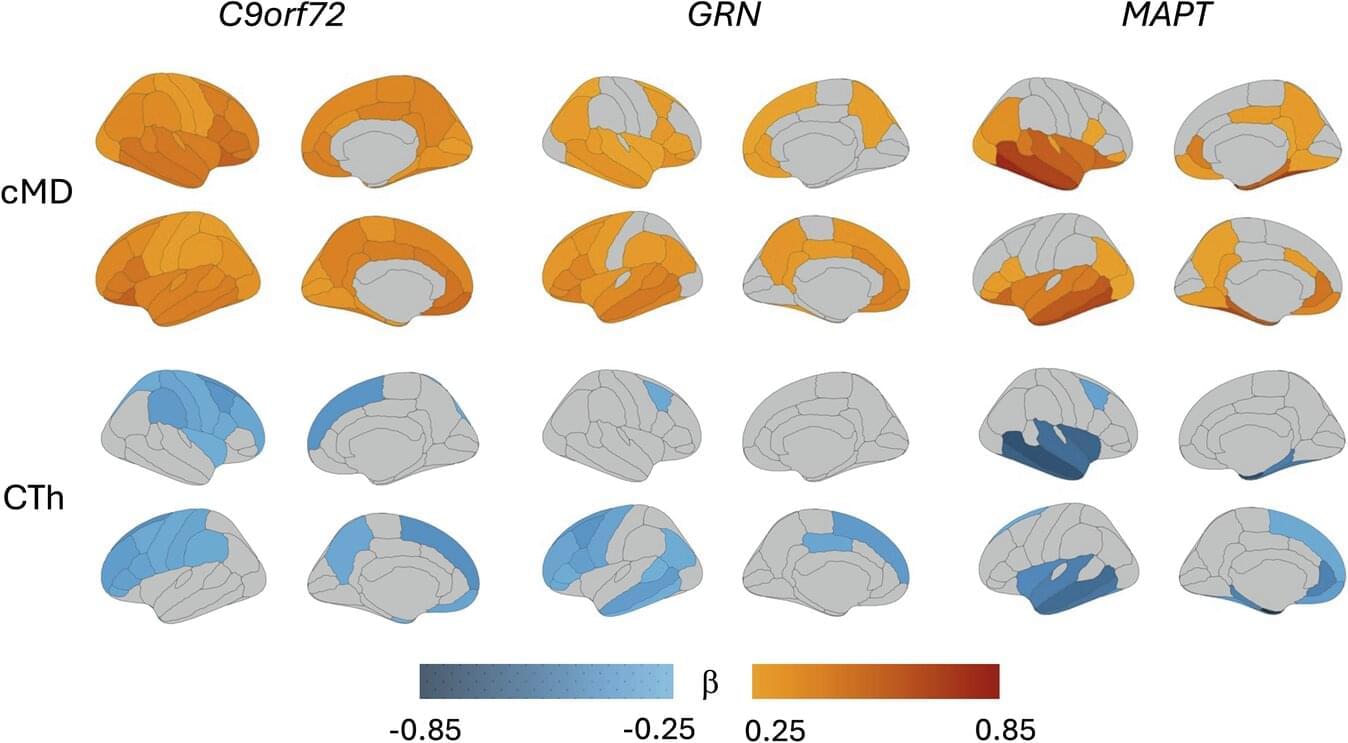
A new international study led by researchers at Karolinska Institutet demonstrates that it is possible to detect subtle changes in the brain and identify early signs of hereditary frontotemporal dementia using advanced brain imaging techniques. The study is published in Molecular Psychiatry.
Frontotemporal dementia, or FTD, is a neurodegenerative disease that often affects people in middle age and is a common cause of dementia before the age of 65. The disease is particularly difficult to diagnose in its early stages, as the earliest symptoms are behavioral changes and may resemble primary psychiatric disease and symptoms later on can resemble conditions such as Alzheimer’s disease and Parkinson’s disease. In about a third of cases, frontotemporal dementia is hereditary, making families with known mutations an important resource for research.
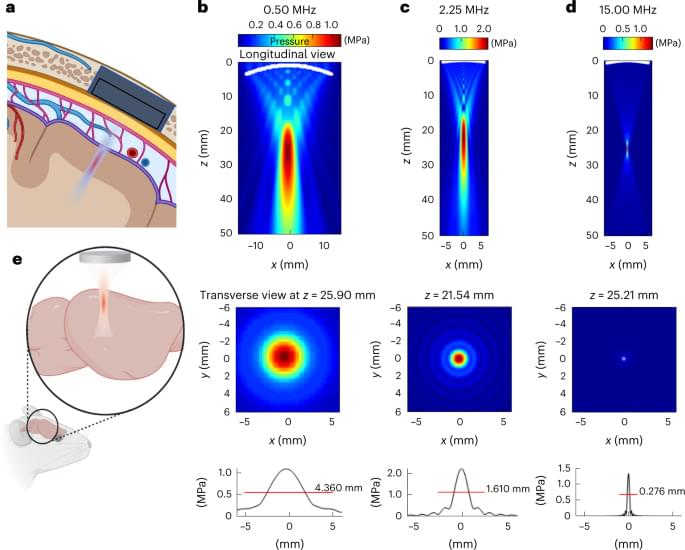
Cadoni et al. show that expression of the bacterial sonogenetic ion channel MscL(G22S) allows focused ultrasound (FUS) neuromodulation of the mouse visual cortex. They even provide evidence for possible induction of a visual percept in mice via this approach, though much more work is needed to make this into a useful visual restoration method. It should be noted that some of the FUS frequencies used in Cadoni et al.’s experiments were quite high (15 MHz), so a surgically implanted cranial window was needed. I personally think that it would be better to focus on frequencies that can be employed in a transcranial fashion to minimize invasiveness. That said, there is still merit to moderately invasive methods as seen here. #sonogenetics [ https://www.nature.com/articles/s41565-023-01359-6](https://www.nature.com/articles/s41565-023-01359-6)
Sonogenetics provides neuron-specific activation at high spatiotemporal resolution ex vivo in retina and in vivo deep in the visual cortex using the AAV gene delivery of a mechanosensitive ion channel and low-intensity ultrasound stimulations.
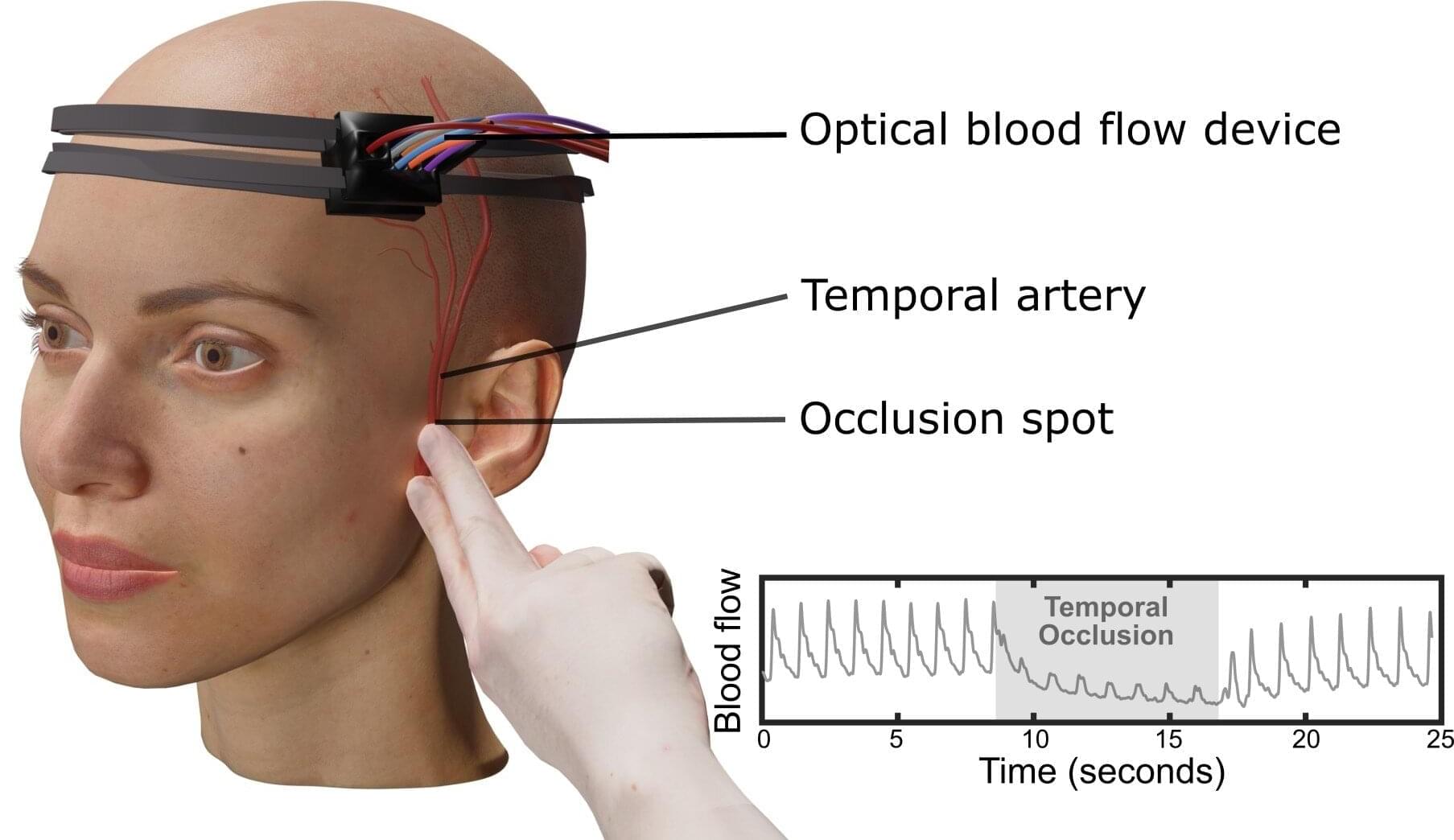
Measuring blood flow in the brain is critical for responding to a range of neurological problems, including stroke, traumatic brain injury (TBI) and vascular dementia. But existing techniques, including magnetic resonance imaging and computed tomography, are expensive and therefore not widely available.
Researchers from the USC Neurorestoration Center and the California Institute of Technology (Caltech) have built a simple, noninvasive alternative. The device takes a technique currently used in animal studies known as speckle contrast optical spectroscopy (SCOS) and adapts it for potential clinical use in humans. It works by capturing images of scattered laser light with an affordable, high-resolution camera.
“It’s really that simple. Tiny blood cells pass through a laser beam, and the way the light scatters allows us to measure blood flow and volume in the brain,” said Charles Liu, MD, Ph.D., professor of clinical neurological surgery, urology and surgery at the Keck School of Medicine of USC, director of the USC Neurorestoration Center and co-senior author of the new research.

