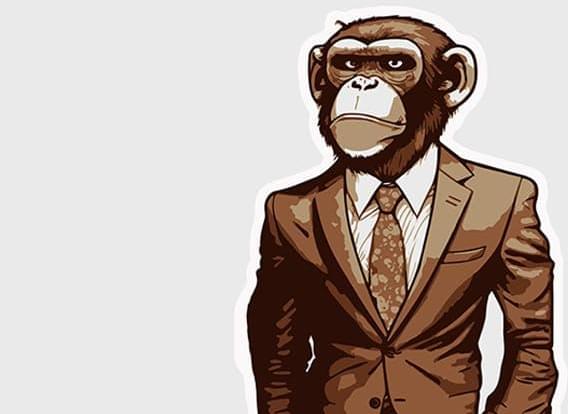
“Rather than seeing the organization as a machine, we need to see it as a collection of clever apes.” Psychologist Robin Dunbar’s latest book argues companies are social groups that can’t be perfected like a machine.
What is it about working life that can make us feel so alienated and isolated, and what can we do to prevent it? In The Social Brain: The Psychology of Successful Groups, the evolutionary psychologist Robin Dunbar joins forces with Tracey Camilleri and Samantha Rockey, associate fellows at Oxford’s Saïd Business School, to apply Dunbar’s own scientific discoveries about human cooperation to our work lives. The idea is that, in order to perform our jobs more effectively, we need to go with, and at times go against, the grain of human nature. The authors home in on what makes us best work together, given the central importance of groups throughout our evolutionary history.
Dunbar spent the better part of two decades, starting in the 1970s, studying wild monkeys in Africa to understand why some species develop their own societies. His close contact with our primate cousins gave him a new perspective from which to approach questions about human nature, and that led him, in 1998, to propose the “social brain hypothesis”—the idea that keeping track of who’s who, and cooperating effectively, takes considerable brain power.