Glioblastoma is one of the deadliest brain cancers, with a median survival rate of just 15 months. Despite surgery and chemotherapy, more than 1250 clinical trials over the past 20 years have struggled to improve survival rates.
Published in Nature Communications, the study shows that a small population of drug-tolerant cells known as “persister cells” rewires its metabolism to survive chemotherapy, using an unexpected ally as an invisibility cloak: a fertility gene called PRDM9.
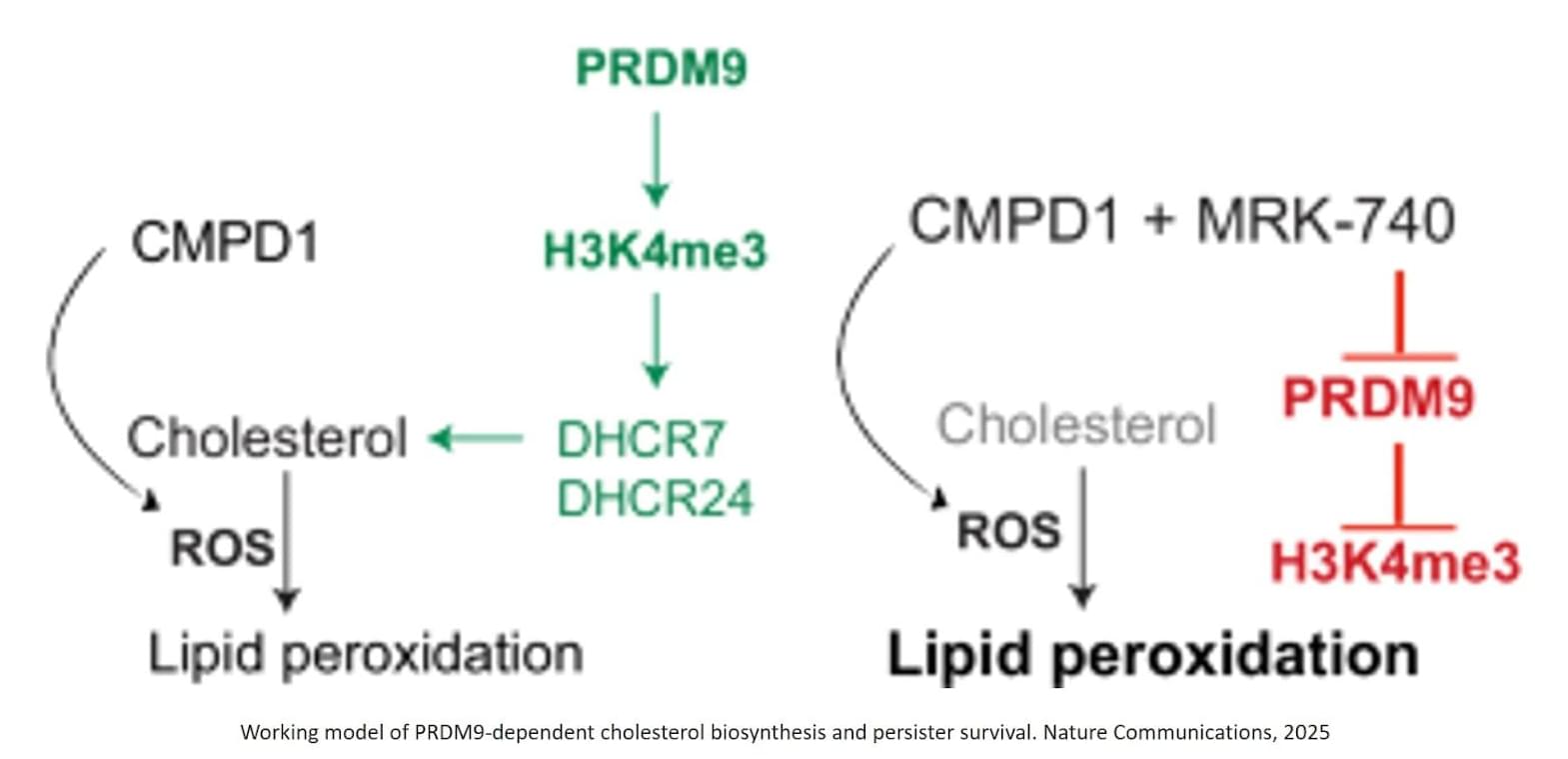
The authors identified that chemotherapy-induced PRDM9 upregulation promotes metabolic rewiring in glioblastoma stem cells, leading to chemotherapy tolerance. Mechanistically, PRDM9-dependent H3K4me3 at cholesterol biosynthesis genes enhances cholesterol biosynthesis, which persister cells rely on to maintain homeostasis under chemotherapy-induced oxidative stress and lipid peroxidation.
PRDM9 inhibition, combined with chemotherapy, results in strong anti-cancer efficacy in preclinical glioblastoma models, significantly enhancing the magnitude and duration of the antitumor response by eliminating persisters.
Previously, PRDM9 was only known as a fertility gene, active in reproductive cells at the very start of egg and sperm formation, long before fertilisation.
The researchers are now working with Australian biotech company Syntara to develop PRDM9 inhibitors for further testing in animal models, with the hope to eventually progress to human studies.