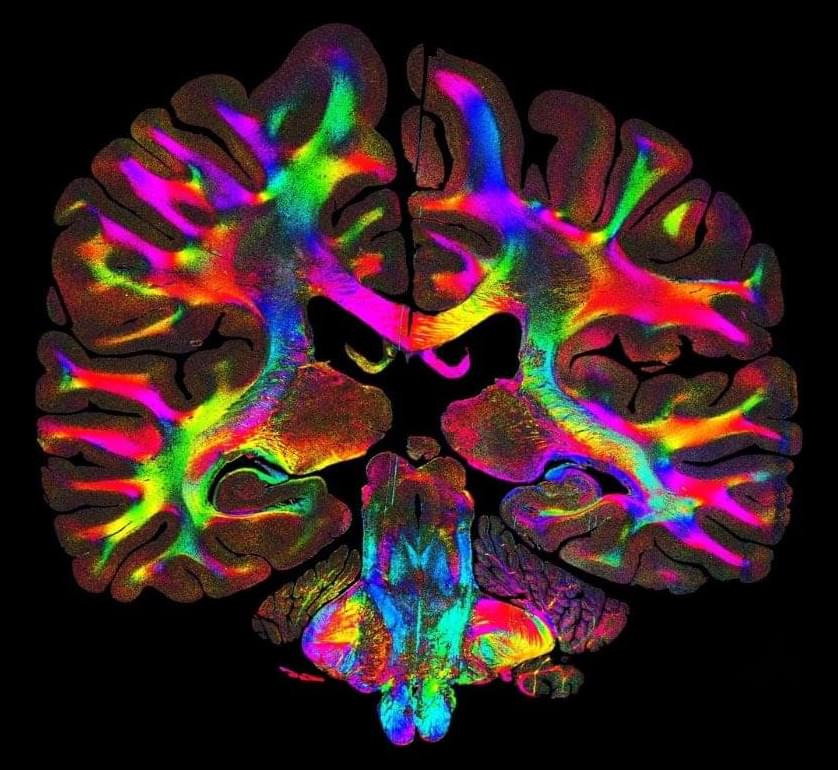
From work meetings to first dates, it’s essential to adjust our behavior for success. In certain situations, it can even be a matter of life or death. So how do we switch our behavior when situations change? Published in Nature Communications, neuroscientists describe the neural basis of behavioral flexibility in mice, with insights which may help us understand a wide variety of diseases and disorders, from addiction to obsessive compulsive disorder (OCD) to Parkinson’s disease.
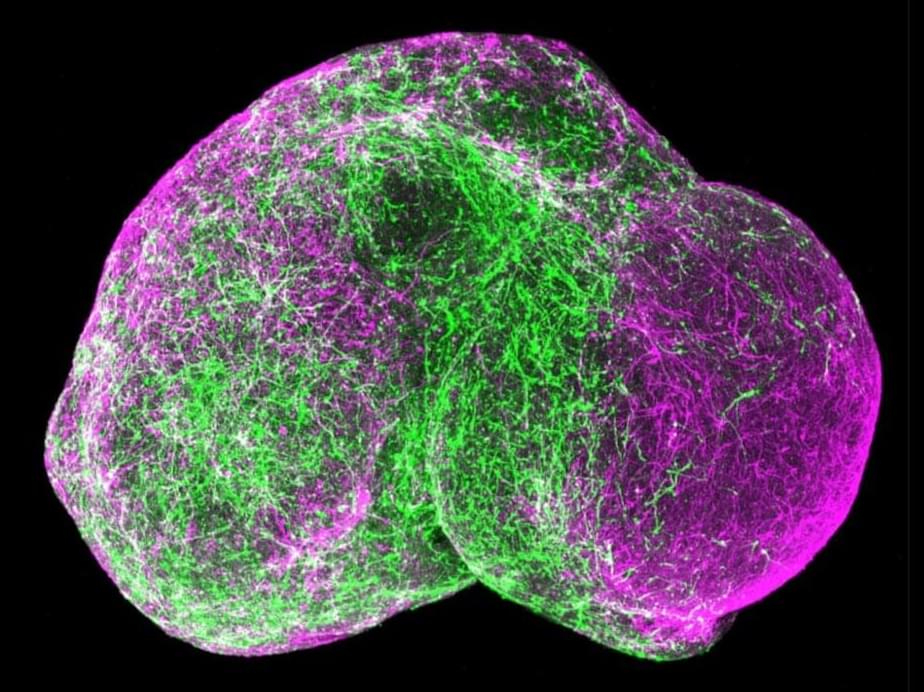
“The brain mechanisms behind changing behaviors have remained elusive, because adapting to a given scenario is very neurologically complex. It requires interconnected activity across multiple areas of the brain,” explains a co-author. “Previous work has indicated that cholinergic interneurons—brain cells that release a neurotransmitter called acetylcholine—are involved in enabling behavioral flexibility. Here, we were able to use advanced imaging techniques to see neurotransmitter release in real time and delve into the fundamental mechanisms behind behavioral flexibility”
In their investigations, the researchers trained mice in a virtual maze, teaching them the correct route to receive a reward. They then switched the route, leading to an unexpected loss of reward for the mice, and observed the effects of this disappointing change using two-photon microscopy.