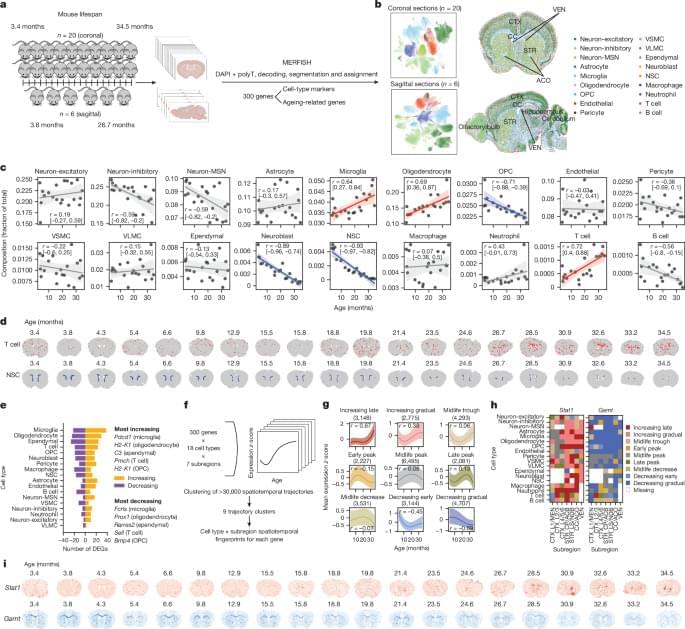
A spatially resolved single-cell transcriptomics map of the mouse brain at different ages reveals signatures of ageing, rejuvenation and disease, including ageing effects associated with T cells and rejuvenation associated with neural stem cells.

Scientists at Neuro-Electronics Research Flanders (NERF), under the direction of Prof. Vincent Bonin, have released two innovative studies that provide fresh perspectives on the processing and distribution of visual information in the brain. These studies contest conventional beliefs regarding the straightforwardness of visual processing, instead emphasizing the intricate and adaptable nature of how the brain understands sensory information.

Thanks to their genetic makeup, their ability to navigate mazes and their willingness to work for cheese, mice have long been a go-to model for behavioral and neurological studies.
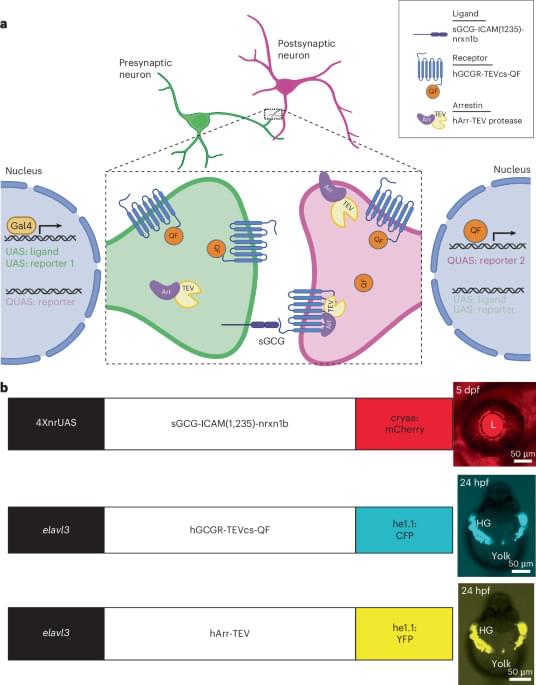
In recent years, they have entered a new arena—virtual reality—and now Cornell researchers have built miniature VR headsets to immerse them more deeply in it.
The team’s MouseGoggles—yes, they look as cute as they sound—were created using low-cost, off-the-shelf components, such as smartwatch displays and tiny lenses, and offer visual stimulation over a wide field of view while tracking the mouse’s eye movements and changes in pupil size.
Summary: Researchers identified variants in the DDX53 gene, located on the X chromosome, as contributors to autism spectrum disorder (ASD). These genetic variants, found predominantly in males, provide critical insights into the biological mechanisms behind autism’s male predominance.
The study also uncovered another potential gene, PTCHD1-AS, near DDX53, linked to autism, emphasizing the complexity of ASD’s genetic architecture. This research highlights the importance of the X chromosome in ASD and opens avenues for more precise diagnostics and therapeutics.
The findings challenge current models, urging a re-evaluation of how autism is studied. These discoveries mark a significant step in understanding the genetic underpinnings of autism.
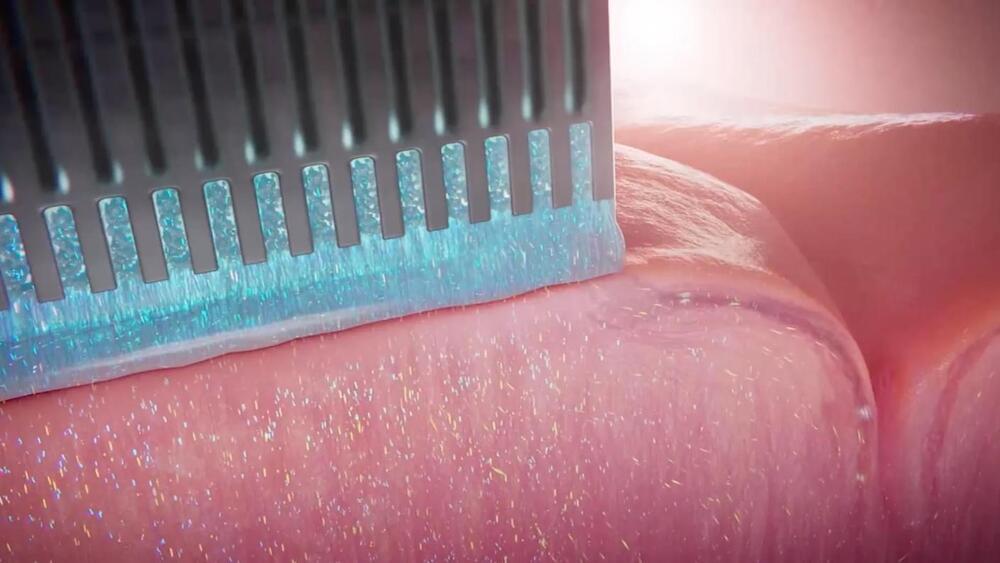
While companies like Neuralink have recently provided some flashy demos of what could be achieved by hooking brains up to computers, the technology still has serious limitations preventing wider use.
Non-invasive approaches like electroencephalograms (EEGs) provide only coarse readings of neural signals, limiting their functionality. Directly implanting electrodes in the brain can provide a much clearer connection, but such risky medical procedures are hard to justify for all but the most serious conditions.
California-based startup Science Corporation thinks that an implant using living neurons to connect to the brain could better balance safety and precision. In recent non-peer-reviewed research posted on bioarXiv, the group showed a prototype device could connect with the brains of mice and even let them detect simple light signals.

For nearly his entire life, Dr. Stuart Hameroff has been fascinated with the bedeviling question of consciousness. But instead of studying neurology or another field commonly associated with the inner workings of the brain, it was Hameroff’s familiarity with anesthetics, a family of drugs that famously induces the opposite of consciousness, that fueled his curiosity.
“I thought about neurology, psychology, and neurosurgery, but none of those… eemed to be dealing with the problem of consciousness,” says Hameroff, a now-retired professor of anesthesiology from the University of Arizona. Hameroff recalls a particularly eye-opening moment when he first arrived at the university and met the chairman of the anesthesia department. “He says ‘hey, if you want to understand consciousness, figure out how anesthesia works because we don’t have a clue.’”
Hameroff’s work in anesthesia showed that unconsciousness occurred due to some effect on microtubules and wondered if perhaps these structures somehow played a role in forming consciousness. So instead of using the neuron, or the brain’s nerve cells, as the “base unit” of consciousness, Hameroff’s ideas delved deeper and looked at the billions of individual tubulins inside microtubules themselves. He quickly became obsessed.


Researchers at University of California San Diego have developed and tested a new software package, called Spatial Modeling Algorithms for Reactions and Transport (SMART), that can realistically simulate cell-signaling networks—the complex systems of molecular interactions that allow cells to respond to diverse cues from their environment.
Cell-signaling networks involve many distinct steps and are also greatly influenced by the complex, three-dimensional shapes of cells and subcellular components, making them difficult to simulate with existing tools. SMART offers a solution to this problem, which could help accelerate research in fields across the life sciences, such as systems biology, pharmacology and biomedical engineering.
The researchers successfully tested the new software in biological systems at several different scales, from cell signaling in response to adhesive cues, to calcium release events in subcellular regions of neurons and cardiac muscle cells, to the production of ATP (the energy currency in cells) within a detailed representation of a single mitochondrion.