Individuals with psychiatric disorders exhibiting seemingly similar symptoms often respond very differently to the same treatment, suggesting that distinct biological processes are at work beneath the surface of similar clinical presentations. Researchers have now identified a distinct immuno-inflammatory biomarker across major psychiatric disorders that can be detected using non-invasive brain imaging. Patients exhibiting this brain signature showed systemic inflammation and poorer response to standard treatments. The findings of the new study in Biological Psychiatry, published by Elsevier, lay the foundation for a biology-augmented diagnostic framework in psychiatry and detail the potential for biomarker-guided, anti-inflammatory precision therapies.
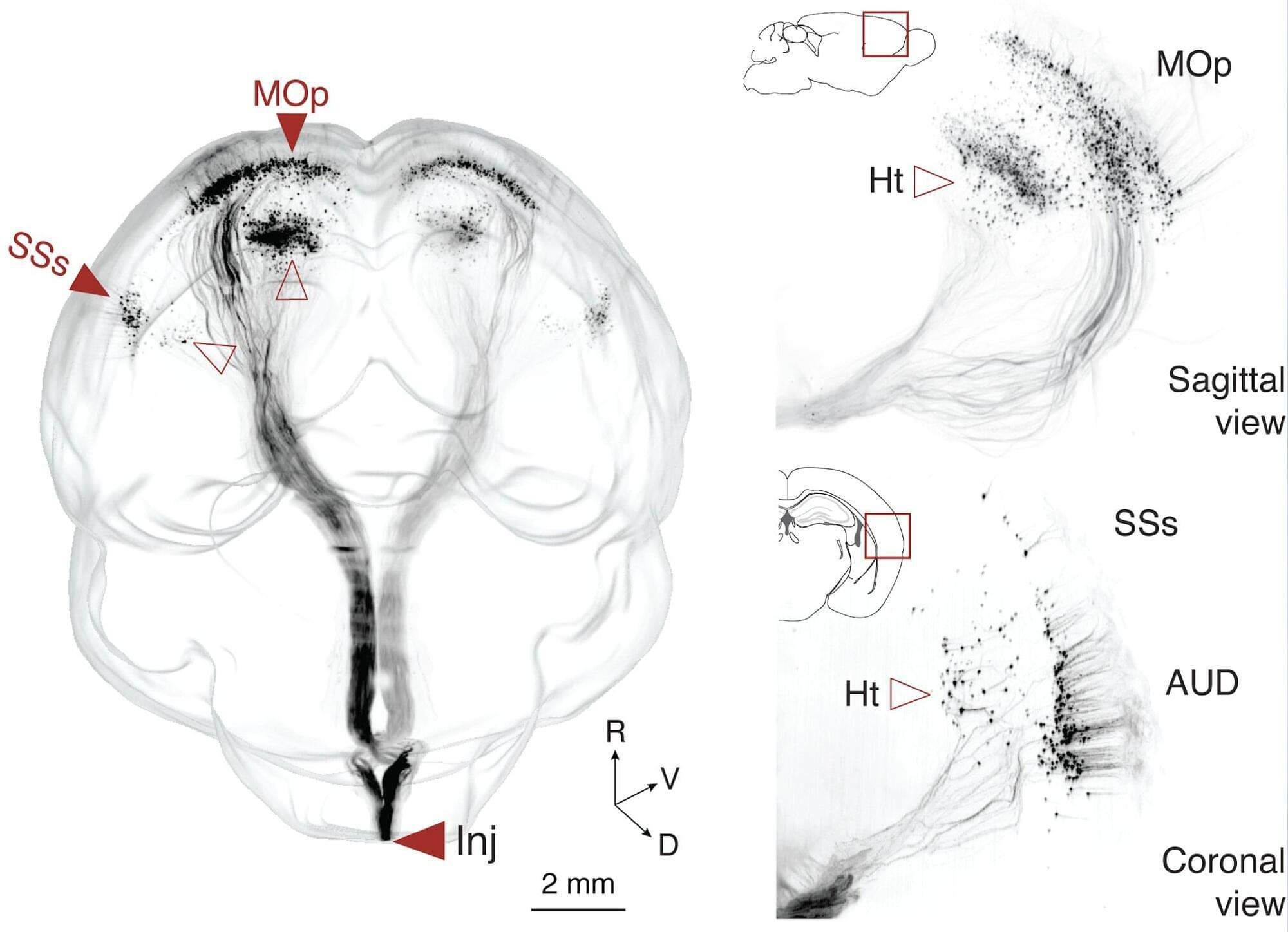
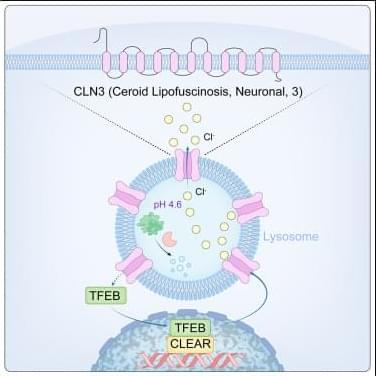
Neuroimaging links diverse biological mechanisms to clinical manifestations, providing compelling insights into the neural mechanisms underlying brain function implicated in psychiatric diseases. Through neuroimaging, shared neural correlates have been increasingly identified across major psychiatric disorders such as schizophrenia, major depressive disorder, and bipolar disorder. While subtypes within and across psychiatric diagnoses have been identified, the biological underpinnings remain unclear. This study aimed to uncover these hidden “biotypes,” focusing particularly on brain inflammation—a mechanism thought to drive illness in a subset of patients, but which is difficult to measure directly in the living brain.
The research was conducted in two independent cohorts. In the first stage, brain connectivity scans were combined with blood-based molecular (DNA methylation) data to identify a brain network pattern linked to immune system dysfunction. In the second longitudinal stage, investigators validated that patients with this brain marker had higher blood inflammation indices—such as neutrophil-to-lymphocyte ratios—and showed less improvement with conventional treatments during hospitalization.