“Historically, this has been a very challenging problem. People don’t know where to start,” said senior author Megan Dennis, associate director of genomics at the UC Davis Genome Center and associate professor in the Department of Biochemistry and Molecular Medicine and MIND Institute at the University of California, Davis.
In 2022, Dennis was a co-author on a paper describing the first sequence of a complete human genome, known as the ‘telomere to telomere’ reference genome. This reference genome includes the difficult regions that had been left out of the first draft published in 2001 and is now being used to make new discoveries.
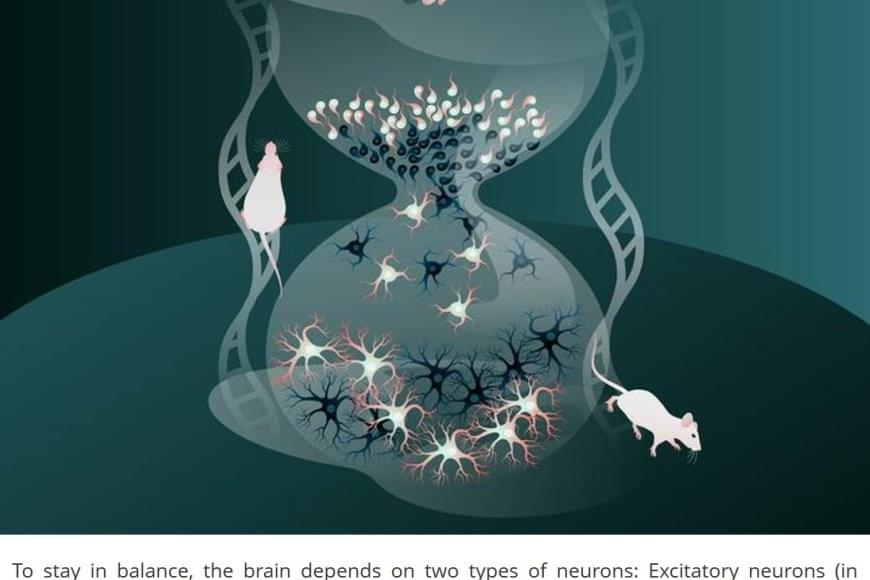
Dennis and colleagues used the telomere-to-telomere human genome to identify duplicated genes. Then, they sorted those for genes that are: expressed in the brain; found in all humans, based on sequences from the 1,000 Genomes Project; and conserved, meaning that they did not show much variation among individuals.
They came out with about 250 candidate gene families. Of these, they picked some for further study in an animal model, the zebrafish. By both deleting genes and introducing human-duplicated genes into zebrafish, they showed that at least two of these genes might contribute to features of the human brain: one called GPR89B led to slightly bigger brain size, and another, FRMPD2B, led to altered synapse signaling.
“It’s pretty cool to think that you can use fish to test a human brain trait,” Dennis said.
The dataset in the Cell paper is intended to be a resource for the scientific community, Dennis said. It should make it easier to screen duplicated regions for mutations, for example related to language deficits or autism, that have been missed in previous genome-wide screening.
“It opens up new areas,” Dennis said.