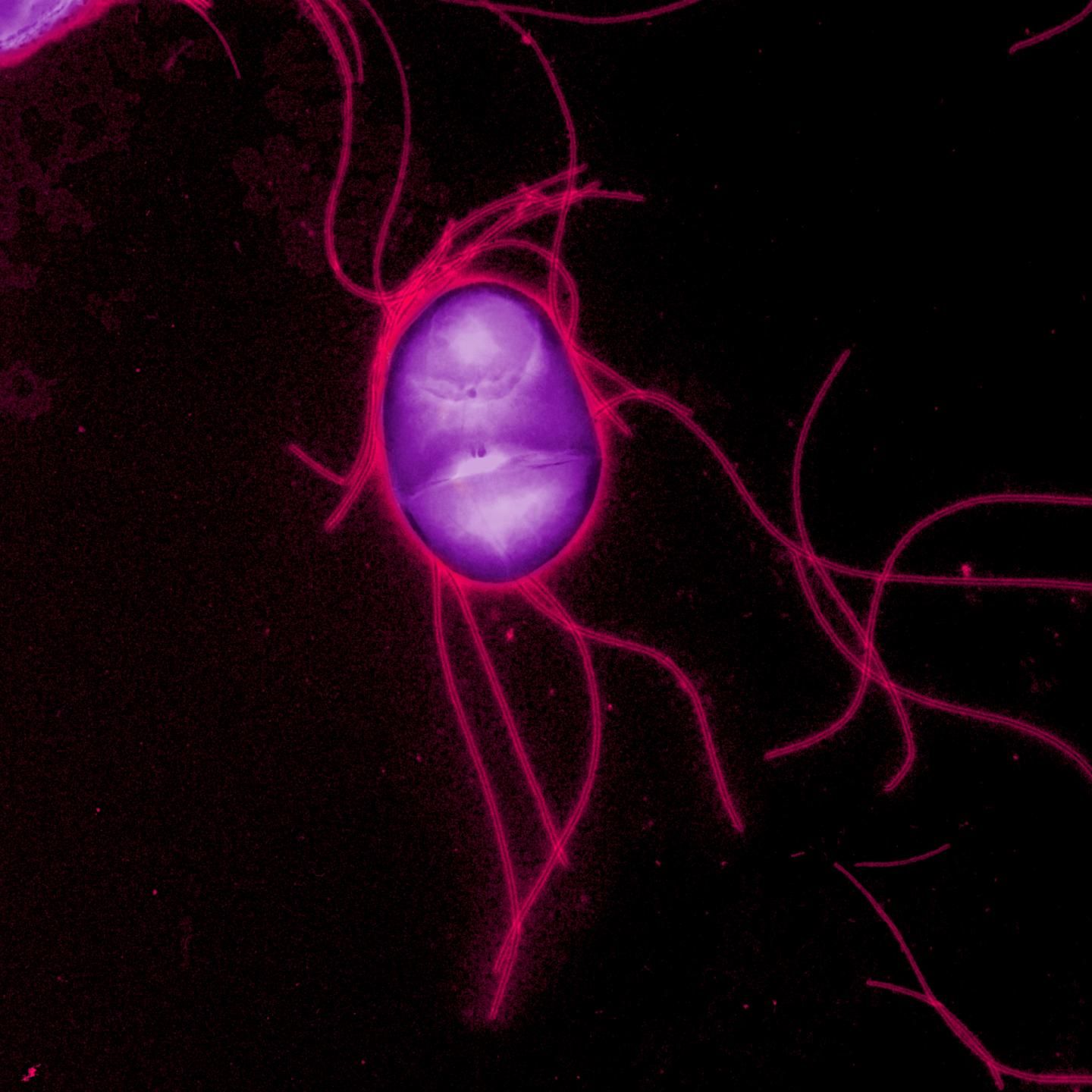
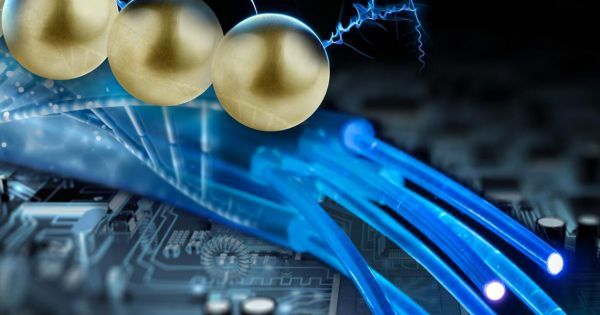
Is Synbio the next big thing? Hmmm; depends. If we’re talking about ensuring that we have a solid foundation/ infrastructure (including platforms; etc.) on QC 1st then with the existing evolution and maturity of the fundamentals around Synbio as a 1st step; then accelerating the further maturity of Synbio into creating super humans and singularity? My answer is yes. If we’re not even considering that we need QC and just focused on Synbio only; my answer is No as QC will be required as a foundation for things like real Humanoid AI, cell circuited humans/ super humans, etc.
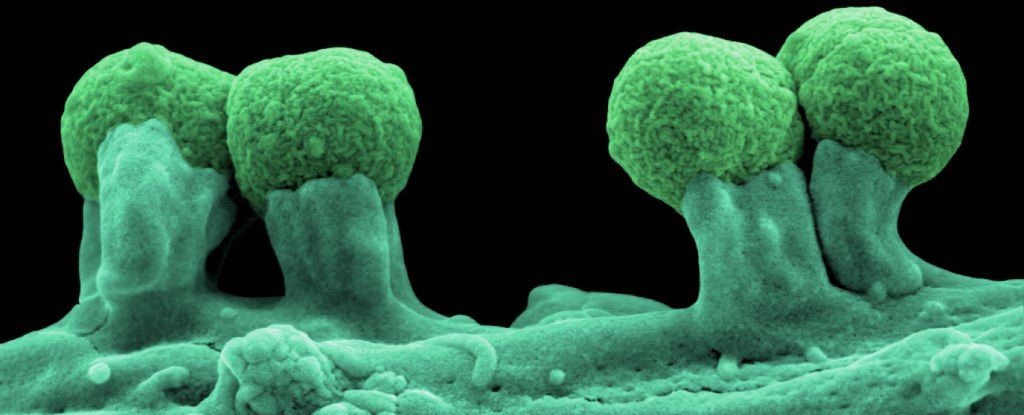
Why we might soon be buying silk, wood, and more fabricated out of genetic code.