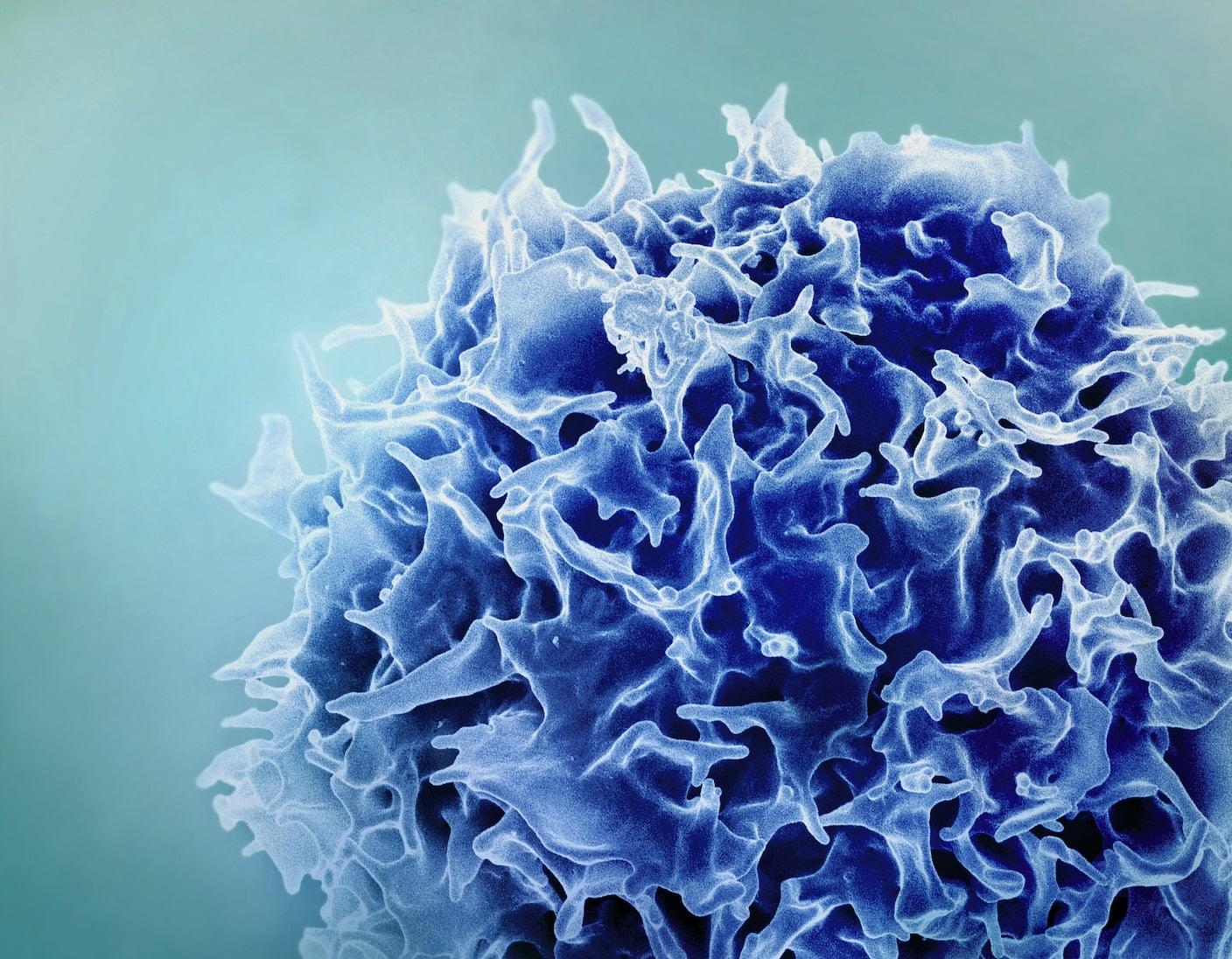
Despite risks, results from both trials highlight the promise of one-and-done CAR T therapy for deadly blood cancers. But it’s still early days. Scientists need to carefully follow patients over years to understand how long upgraded T cells remain in the body and their effect on cancers.
And not all viral carriers are made the same. Lentiviruses, used in both studies, can tunnel into the human genome, causing DNA typos that potentially trigger secondary cancers. The durability of the therapy, its longevity, and immune side effects also need to be studied.
Kelonia is adding more patients to their trial, amid an increasingly competitive landscape. AstraZeneca has acquired EsoBiotec to bring its technology to market. AbbVie, a drug company in Illinois, is testing the delivery of gene-editing tools to T cells via fatty nanoparticles in clinical trials. And Kelonia is planning a second clinical trial with an initial 20 patients and 20 more in an expansion phase, none of whom responded to at least three previous treatments.