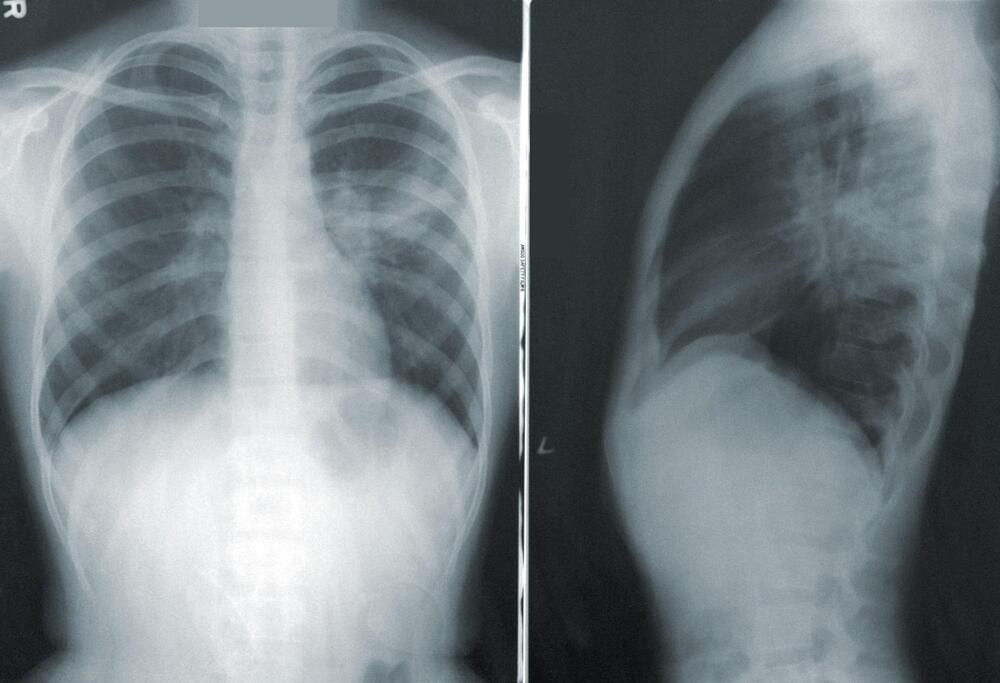
For decades, scientists and pathologists have tried, without much success, to come up with a way to determine which individual lung cancer patients are at greatest risk of having their illness spread, or metastasize, to other parts of the body.
Now a team of scientists from Caltech and the Washington University School of Medicine in St. Louis has fed that problem to artificial intelligence (AI) algorithms, asking computers to predict which cancer cases are likely to metastasize. In a novel pilot study of non-small cell lung cancer (NSCLC) patients, AI outperformed expert pathologists in making such predictions.
These predictions about the progression of lung cancer have important implications in terms of an individual patient’s life. Physicians treating early-stage NSCLC patients face the extremely difficult decision of whether to intervene with expensive, toxic treatments, such as chemotherapy or radiation, after a patient undergoes lung surgery. In some ways, this is the more cautious path because more than half of stage I–III NSCLC patients eventually experience metastasis to the brain. But that means many others do not. For those patients, such difficult treatments are wholly unnecessary.