Melanoma, the most dangerous type of skin cancer, remains in the top five cancers diagnosed in both men and women. Scientists understand that most melanoma cells express antigens, proteins that prompt the body to initiate an immune response. We consider these antigens “unique” because other non-melanoma cells do not usually express them. Thus, melanoma antigens present a viable target for cancer treatment.
However, melanoma vaccines made to target antigens remain limited in clinical efficacy. One potential opportunity for cancer vaccines involves the antigens targeted by a particular vaccine. While original vaccines targeted one or two antigens, studies have shown that vaccines that recognize up to 12 antigens elicit a more robust immune response.
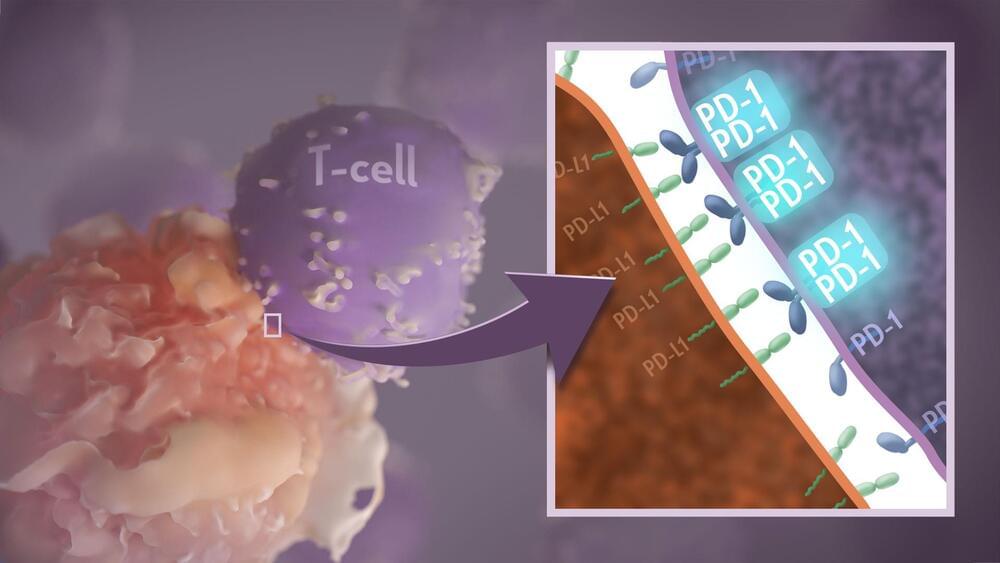
Still, vaccine development has continued to evolve to improve clinical efficacy. One area of focus concerns the type of immune cells elicited by the vaccine. CD8+ T cells, the immune cells that kill cancer cells, represent the most critical type of immune cell needed for an effective anti-tumor immune response. However, during an immune response, CD4+ T cells, also known as “helper” T cells, stimulate CD8+ T cells. In other words, CD4+ T cells “help” CD8+ T cells become activated and eliminate cancer cells.