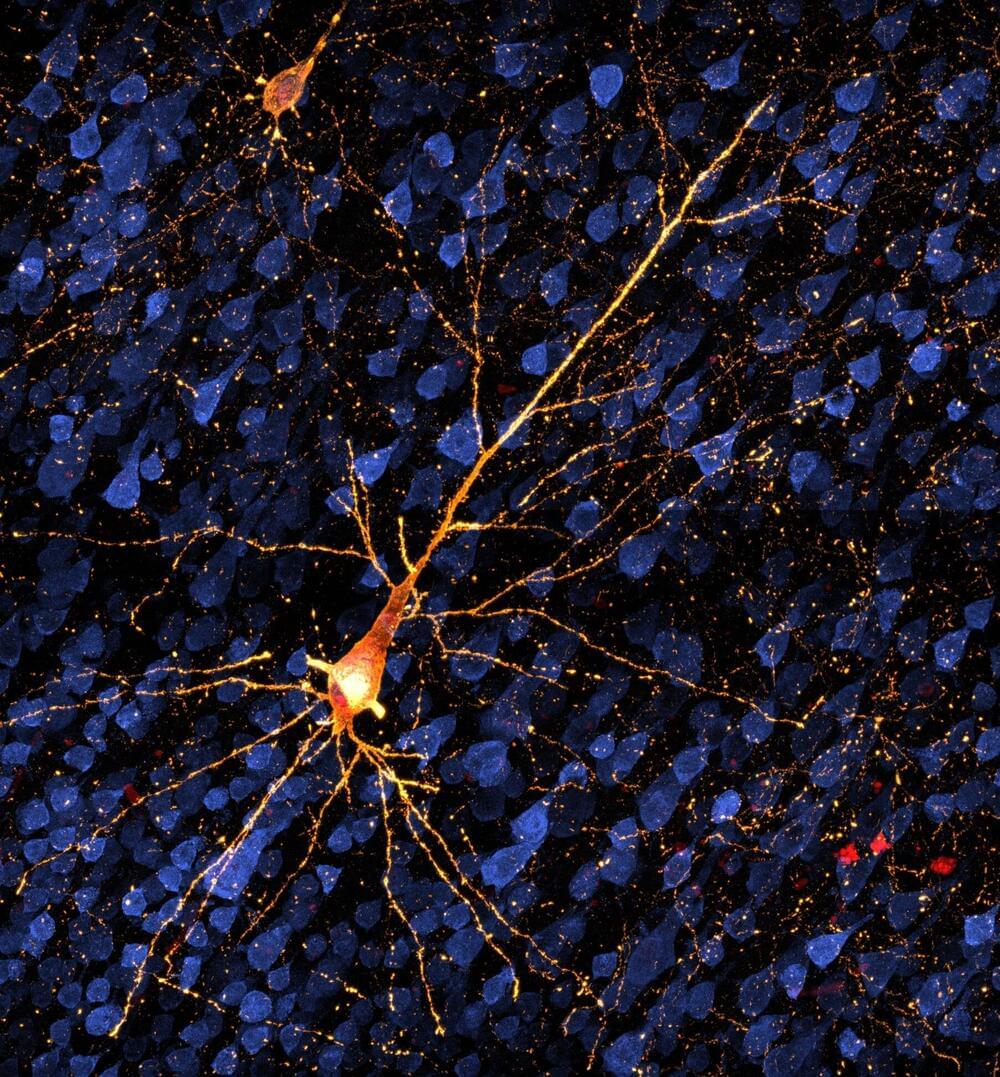
A UK teenager with severe epilepsy has become the first person in the world to be fitted with a brain implant aimed at bringing seizures under control.
Oran Knowlson’s neurostimulator sits under the skull and sends electrical signals deep into the brain, reducing his daytime seizures by 80%.
His…
His mother, Justine, said that her son had been happier, chattier and had a much better quality of life since receiving the device. “The future looks hopeful, which I wouldn’t have dreamed of saying six months ago,” she said.
Martin Tisdall, a consultant paediatric neurosurgeon who led the surgical team at Great Ormond Street hospital (Gosh) in London, said: “For Oran and his family, epilepsy completely changed their lives and so to see him riding a horse and getting his independence back is absolutely astounding. We couldn’t be happier to be part of their journey.”
Oran, who is 13 and lives in Somerset, had the surgery in October as part of a trial at Gosh in partnership with University College London, King’s College hospital and the University of Oxford. Oran has Lennox-Gastaut syndrome, external, a treatment-resistant form of epilepsy which he developed at the age of three.