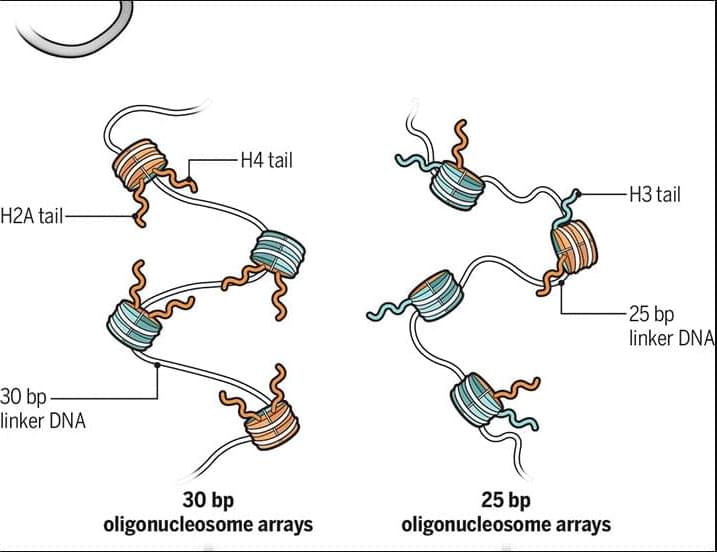
For Louis-Jan Pilaz, days spent with tools and wood began as simple home improvement projects. He soon found himself learning how to whittle scraps of wood. Then, as a neurobiologist, Pilaz noticed a striking parallel. “It made so much sense to use wood to render neurons…They look like trees, and they have this flow of energy that is just like in neurons.” Inspired, he began to shape wood into intricate neural forms, transforming casual whittling into science-inspired woodworking art.
When he first shared his artwork on X (then Twitter), the response was positive, and people expressed their interest in his work. Encouraged by his graduate student, Pilaz opened an Etsy shop in 2021 to sell his wood sculptures, and NeuroWoodworks was born.
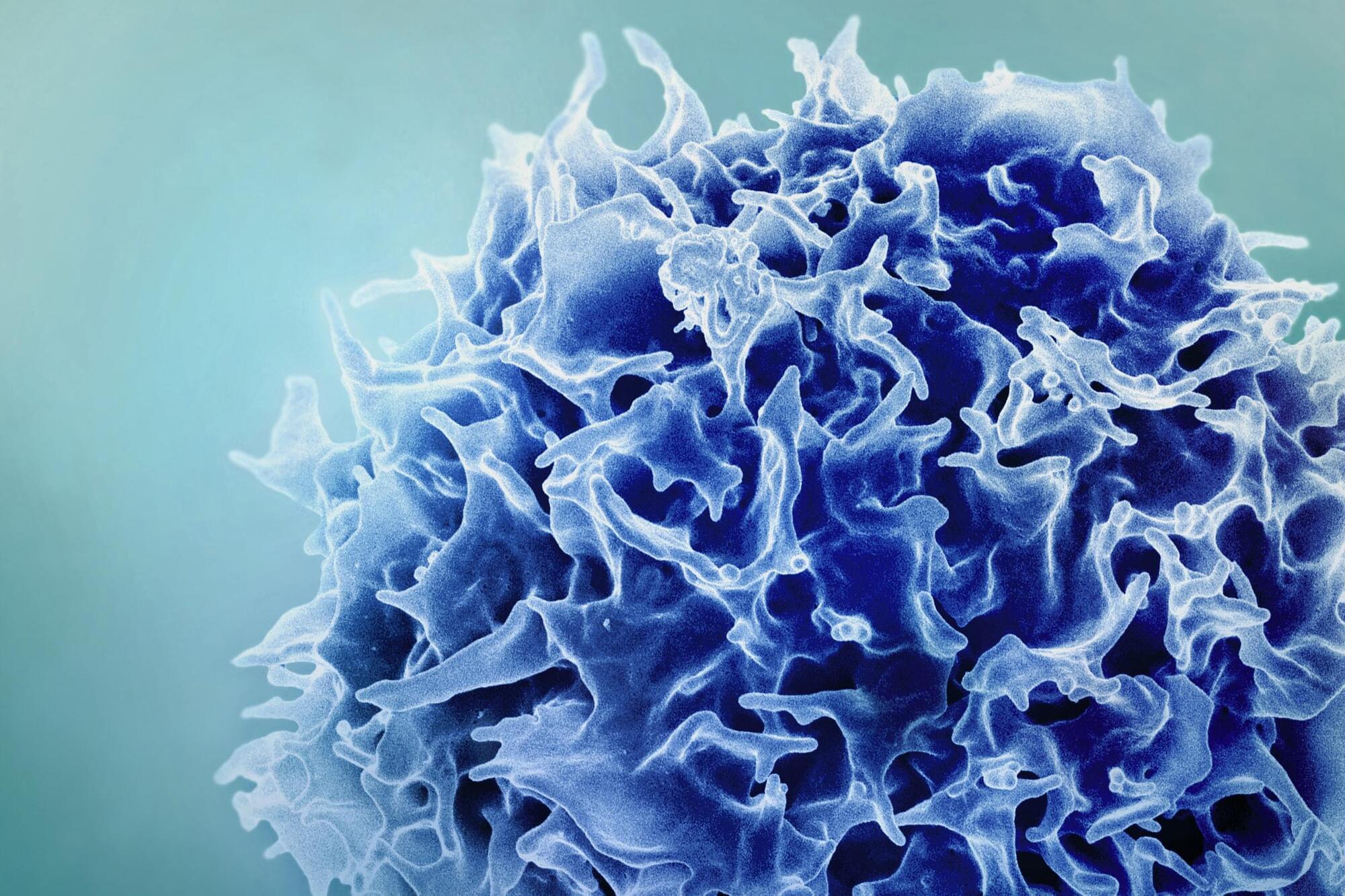
Pilaz’s group at Sanford Research studies the development and dysfunction of the cerebral cortex and makes extensive use of microscopy, which fuels his research and serves as a source of inspiration for his wood art. “I’ve been obsessed with cell morphology since my PhD,” Pilaz said. “I experimented, just like I do in the lab, with the tools I have and tried to make [different cell] shapes.” He uses different types of wood, such as walnut and padauk, to create a variety of cell types and structures from Purkinje cells and radial glia to mitochondria.