Two forgotten bottles in a basement in Frederiksberg containing bacterial cultures from the 1890s have provided researchers at the University of Copenhagen with unique insight into Denmark’s butter production history. Using advanced DNA analysis, they have examined the contents of the bottles, which offered several bacterial surprises and a reminder of the challenges of hygiene at the time.
Lactic acid bacteria have long been used to flavor food and extend its shelf life by acidifying it and displacing harmful bacteria. Denmark was among the first to use the magic of lactic acid bacteria industrially, which, together with the introduction of pasteurization, helped to ensure the high quality of dairy products and, not least, keep them free of disease.
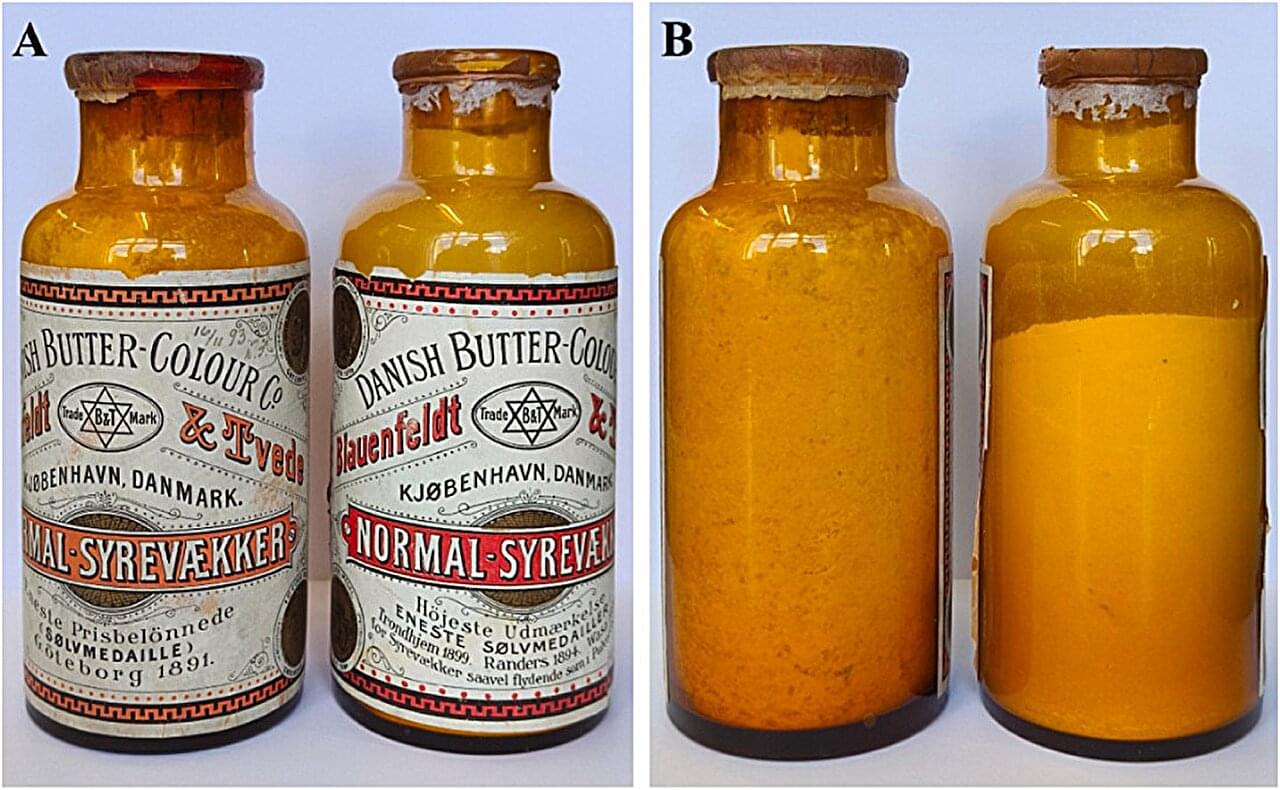
This is evidenced by the discovery of two bottles of white powder, which researchers from the University of Copenhagen found by chance in a dusty moving box last year. The bottles had labels indicating that they contained cultures consisting of lactic acid bacteria, but had not seen the light of day since the late 1800s and were well hidden away in a basement under the greenhouses on Rolighedsvej near the old Agricultural College in Frederiksberg.