Stores of glucose in the brain could play a much more significant role in the pathological degeneration of neurons than scientists realized, opening the way to new treatments for conditions like Alzheimer’s disease.
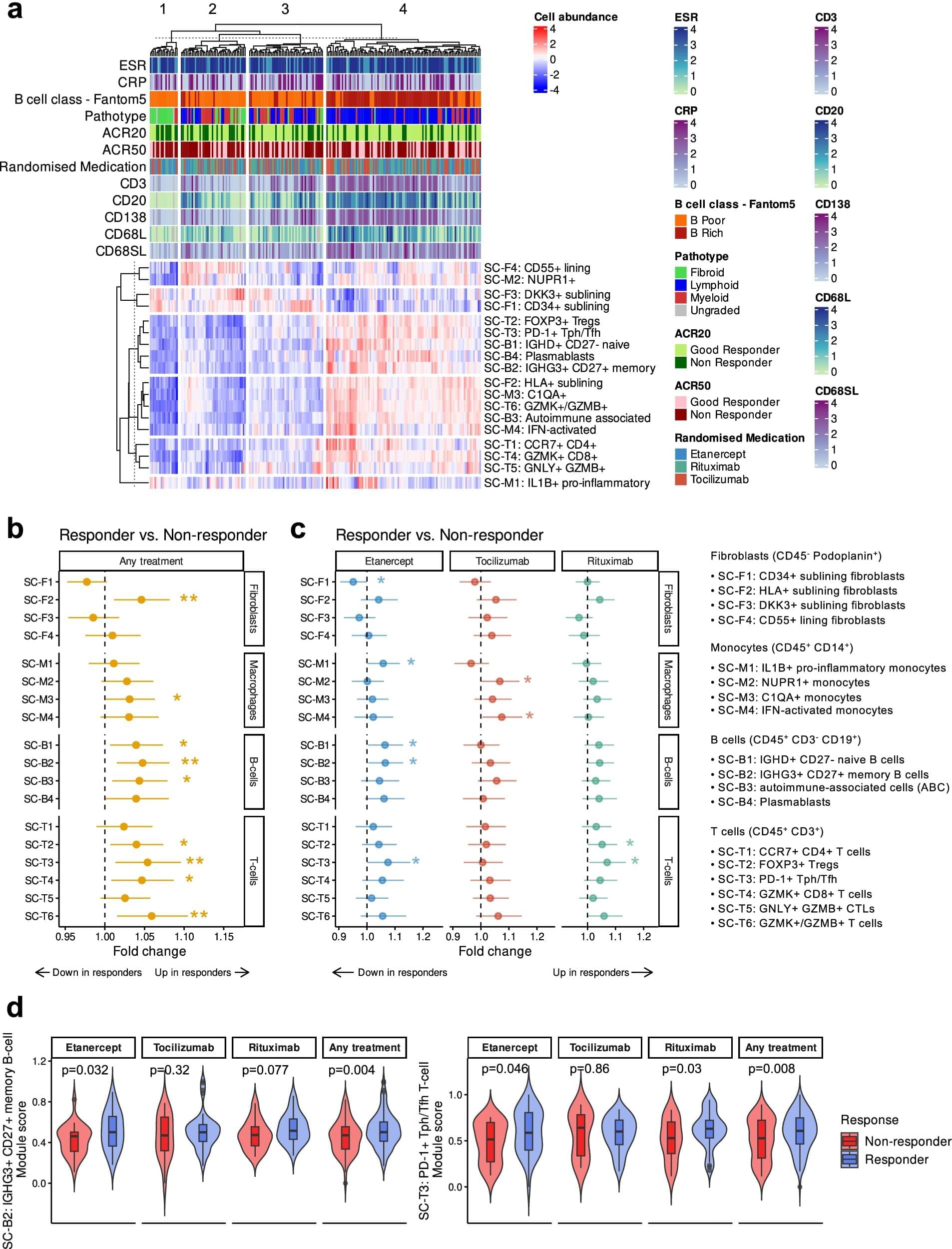
Alzheimer’s is a tauopathy; a condition characterized by harmful build-ups of tau proteins inside neurons. It’s not clear, however, if these build-ups are a cause or a consequence of the disease. A new study now adds important detail by revealing significant interactions between tau and glucose in its stored form of glycogen.
Led by a team from the Buck Institute for Research on Aging in the US, the research sheds new light on the functions of glycogen in the brain. Before now, it’s only been regarded as an energy backup for the liver and the muscles.