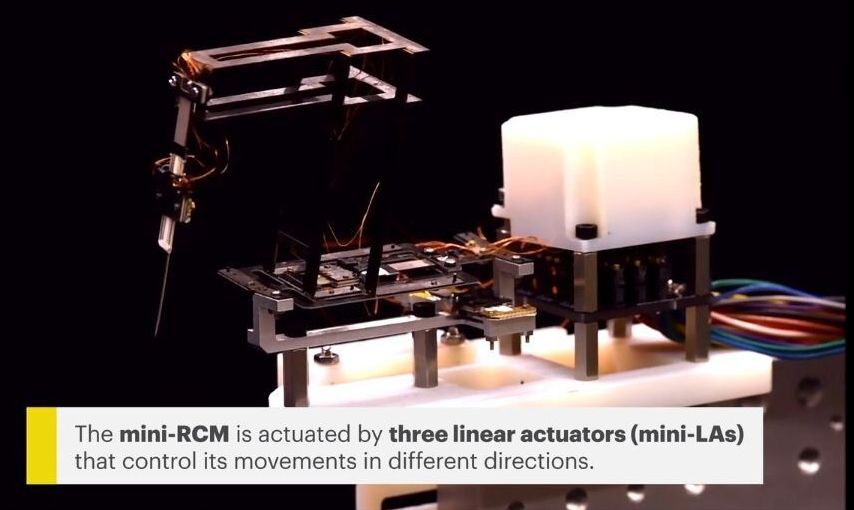
Light, sound, and now, heat — just as optical invisibility cloaks can bend and diffract light to shield an object from sight, and specially fabricated acoustic metamaterials can hide an object from sound waves, a recently developed thermal cloak can render an object thermally invisible by actively redirecting incident heat.
The system, designed by by scientists at the Nanyang Technological University (NTU) in Singapore, has the potential to fine-tune temperature distribution and heat flow in electronic and semiconductor systems. It has application in devices with high requirements for efficient dissipation and homogenous thermal expansion, such as high-power engines, magnetic resonance imaging (MRI) instruments, and thermal sensors.
“Because of its shape flexibility, the active thermal cloak might also be applied in human garments for effective cooling and warming, which makes a lot of sense in tropical areas such as Singapore,” said Prof. Baile Zhang of NTU.