Circa 2019.
Gain of function research was heavily debated amidst many CDC mishaps. It was stopped, and then outsourced to China due to lax regulations. Now we have an outbreak that no one can confirm it’s origin, but the epicenter is in close proximity to a Wuhan lab working on the same pathogen, with direct bat to human transmission.
Knowing this, this story disturbs me, as we have no international protocols and regulations to prevent mishaps. The last thing we need is a lab mishap, and monkeys riding on horses with guns, all pissed off at humans. We are already experiencing the Contagion movie, and biblical plagues like locusts, the last we need is planet of the apes.
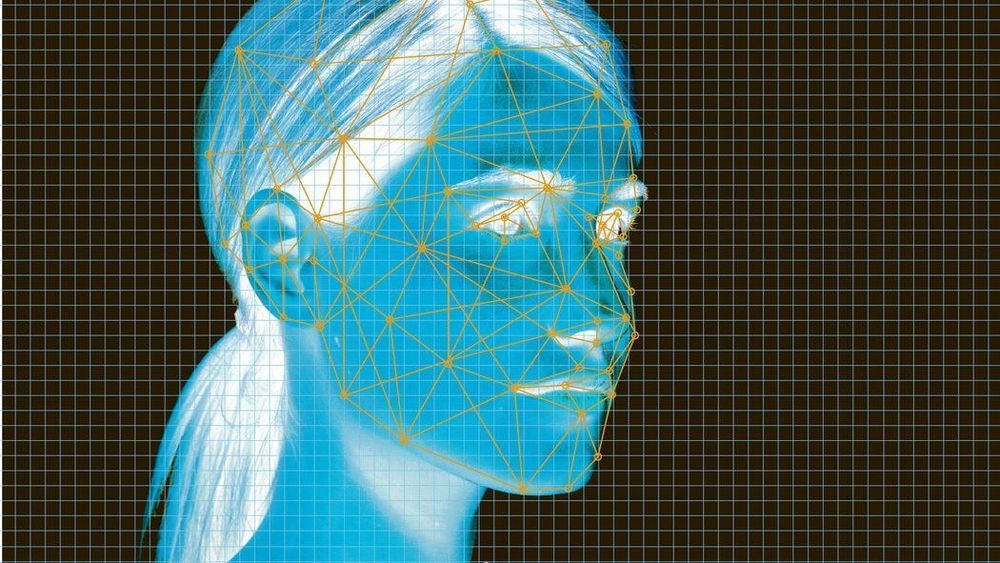
In a controversial first, a team of researchers have been creating embryos that are part human and part monkey, reports the Spanish daily El País.
Daring biologist: According to the newspaper, the Spanish-born biologist Juan Carlos Izpisúa Belmonte, who operates a lab at the Salk Institute in California, has been working working with monkey researchers in China to perform the disturbing research.
Their objective is to create “human-animal chimeras,” in this case monkey embryos to which human cells are added.